Table of Contents
ToggleA Comprehensive Guide for Nursing Students

Evidence-based practice (EBP) has become the cornerstone of modern nursing education and clinical practice. As we advance into 2025, nursing students face the challenge of selecting relevant, impactful topics for their EBP assignments that reflect current healthcare trends and address pressing patient care needs. This comprehensive guide presents the most current and relevant evidence-based practice nursing topics, designed to help students excel in their academic pursuits while contributing meaningfully to healthcare outcomes.
Understanding Evidence-Based Practice in Nursing
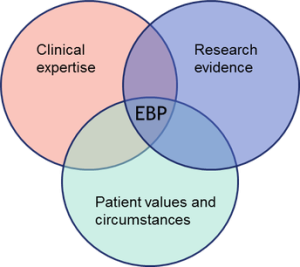
Evidence-based practice in nursing integrates the best available research evidence with clinical expertise and patient values to make informed decisions about patient care. For nursing students, EBP assignments serve as crucial learning tools that bridge theoretical knowledge with practical application, preparing them for real-world clinical scenarios.
The significance of EBP in nursing cannot be overstated. According to recent healthcare statistics, hospitals implementing evidence-based practices report 15-20% improvement in patient outcomes and 10-15% reduction in healthcare costs. This makes EBP topic selection critical for both academic success and future professional impact.
Top Evidence-Based Practice Nursing Topics for 2025
1. Digital Health and Technology Integration
Primary Focus Areas:
- Telehealth implementation in rural healthcare settings
- AI-assisted clinical decision-making tools
- Electronic health record optimization
- Mobile health applications for chronic disease management

Research Questions:
- How does telehealth implementation affect patient satisfaction in rural communities?
- What is the impact of AI diagnostic tools on nursing workflow efficiency?
- How do mobile health apps improve medication adherence in diabetic patients?
2. Mental Health and Psychiatric Nursing
Critical Topics:
- Post-pandemic mental health interventions
- Trauma-informed care in emergency departments
- Suicide prevention strategies in healthcare settings
- Mental health screening protocols in primary care
Statistics: Mental health-related emergency department visits increased by 25% post-2020, making this area particularly relevant for EBP research.
3. Infection Control and Prevention
Key Areas:
- Antimicrobial resistance prevention strategies
- Hand hygiene compliance improvement methods
- Isolation protocol effectiveness
- Healthcare-associated infection reduction techniques
Research Focus:
- Effectiveness of educational interventions on hand hygiene compliance
- Impact of antimicrobial stewardship programs on resistance rates
- Comparative analysis of isolation protocols across different healthcare settings
4. Geriatric and Aging Population Care

Essential Topics:
- Fall prevention strategies in elderly care facilities
- Dementia care best practices
- Polypharmacy management in older adults
- Age-friendly healthcare environment design
Supporting Data: By 2025, adults aged 65+ will comprise 20% of the U.S. population, making geriatric care EBP topics increasingly relevant.
5. Pediatric and Neonatal Nursing
Focus Areas:
- Pain management in pediatric patients
- Family-centered care implementation
- Neonatal intensive care unit best practices
- Childhood obesity prevention programs
Research Opportunities:
- Effectiveness of non-pharmacological pain management in children
- Impact of family presence during medical procedures
- Comparative analysis of feeding protocols in NICUs
Evidence-Based Practice Topics by Specialty Areas
Medical-Surgical Nursing
| Topic Category | Specific Research Areas | Evidence Level |
|---|---|---|
| Wound Care | Negative pressure therapy effectiveness | Level I |
| Post-operative Care | Early mobilization protocols | Level I |
| Medication Administration | Barcode scanning impact on errors | Level II |
| Patient Education | Discharge planning effectiveness | Level II |
Emergency Nursing
High-Impact Topics:
- Triage accuracy improvement methods
- Sepsis recognition and early intervention
- Emergency department overcrowding solutions
- Trauma care protocol standardization
Research Statistics: Emergency departments implementing evidence-based triage protocols report 30% reduction in patient wait times and 20% improvement in patient satisfaction scores.
Critical Care Nursing

Priority Areas:
- Ventilator-associated pneumonia prevention
- Delirium assessment and management
- Family communication in ICU settings
- End-of-life care protocols
Community Health Nursing
Relevant Topics:
- Health promotion program effectiveness
- Chronic disease management in communities
- Healthcare access improvement strategies
- Cultural competency in healthcare delivery
Easy EBP Nursing Topics for Beginners
For nursing students new to evidence-based practice research, these topics provide manageable scope while maintaining academic rigor:
Beginner-Friendly Research Areas
- Hand Hygiene Compliance
- Scope: Single unit or department
- Methodology: Observational study with intervention
- Timeline: 4-6 weeks
- Patient Fall Prevention
- Focus: Specific fall prevention protocol
- Measurement: Fall rates before and after intervention
- Setting: Medical-surgical unit
- Medication Error Reduction
- Intervention: Double-checking protocols
- Outcome: Error rate comparison
- Duration: 8-week study period
- Patient Education Effectiveness
- Topic: Discharge instruction comprehension
- Method: Pre/post-test design
- Population: Specific patient group
Advanced EBP Topics for Graduate Students

Complex Research Areas
Multi-System Interventions:
- Interprofessional collaboration impact on patient outcomes
- Healthcare system redesign for chronic disease management
- Quality improvement initiatives across multiple departments
Population Health Focus:
- Social determinants of health impact studies
- Healthcare equity improvement strategies
- Community-based intervention effectiveness
Research Methodology Considerations
Quantitative Research Approaches
| Research Design | Best Applied To | Strength of Evidence |
|---|---|---|
| Randomized Controlled Trial | Intervention effectiveness | Highest |
| Cohort Study | Long-term outcomes | High |
| Case-Control Study | Risk factor identification | Moderate |
| Cross-sectional Survey | Current practice assessment | Moderate |
Qualitative Research Methods
When to Use:
- Understanding patient experiences
- Exploring healthcare provider perspectives
- Investigating cultural factors in care delivery
- Examining barriers to implementation
Current Healthcare Trends Influencing EBP Topics
Post-Pandemic Healthcare Priorities
- Infection Control Enhancement
- Personal protective equipment optimization
- Visitor policy effectiveness
- Remote monitoring implementation
- Workforce Resilience
- Nurse burnout prevention strategies
- Staffing model effectiveness
- Professional development impact
- Healthcare Delivery Innovation
- Hybrid care models
- Remote patient monitoring
- AI-assisted clinical decision-making
Emerging Technology Integration
Priority Areas:
- Wearable device data utilization
- Predictive analytics in patient care
- Virtual reality in nursing education
- Robotic assistance in clinical settings
Topic Selection Guidelines
Assessment Criteria
When selecting evidence-based practice topics, consider these essential factors:
- Clinical Relevance
- Addresses current healthcare challenges
- Impacts patient outcomes
- Applicable to practice setting
- Research Feasibility
- Available resources and time
- Access to study population
- Ethical considerations
- Evidence Availability
- Sufficient literature base
- Recent research publications
- Diverse study designs
- Personal Interest
- Aligns with career goals
- Matches specialty interests
- Sustainable motivation
Implementation Strategies
Successful EBP Project Development
Phase 1: Planning (Weeks 1-2)
- Literature review completion
- Methodology selection
- Resource identification
Phase 2: Implementation (Weeks 3-8)
- Data collection
- Intervention delivery
- Progress monitoring
Phase 3: Evaluation (Weeks 9-10)
- Data analysis
- Outcome assessment
- Recommendation development
Common Challenges and Solutions
| Challenge | Solution Strategy |
|---|---|
| Limited time | Focus on single-unit studies |
| Resource constraints | Utilize existing data sources |
| Access barriers | Partner with clinical sites |
| Scope too broad | Narrow to specific population |
Quality Improvement Integration
Linking EBP to QI Initiatives
Evidence-based practice assignments can directly contribute to quality improvement efforts by:
- Identifying best practices for implementation
- Measuring intervention effectiveness
- Providing data for policy development
- Supporting accreditation requirements
Measurement and Outcomes
Key Performance Indicators:
- Patient satisfaction scores
- Clinical outcome metrics
- Cost-effectiveness measures
- Staff compliance rates
Future Directions in EBP Nursing Research
Emerging Research Areas
- Precision Medicine Integration
- Personalized care protocols
- Genetic testing implications
- Targeted therapy effectiveness
- Sustainability in Healthcare
- Environmental impact reduction
- Resource optimization strategies
- Green healthcare initiatives
- Global Health Perspectives
- Cultural adaptation of interventions
- Healthcare equity improvement
- International collaboration models
Conclusion
Evidence-based practice remains fundamental to advancing nursing knowledge and improving patient care outcomes. The topics presented in this guide reflect current healthcare priorities while providing diverse options for nursing students at various academic levels. Success in EBP assignments requires careful topic selection, rigorous methodology, and practical application of findings.
As healthcare continues to evolve, nursing students must remain committed to evidence-based approaches that prioritize patient safety, care quality, and professional excellence. The investment in EBP education today directly translates to improved patient outcomes and healthcare system effectiveness tomorrow.
By selecting relevant, well-researched topics and following systematic implementation strategies, nursing students can contribute meaningfully to healthcare advancement while developing essential skills for professional practice. The future of nursing depends on practitioners who can critically evaluate evidence, implement best practices, and continuously improve care delivery through research-informed decision-making.
Additional Resources
Professional Organizations
- American Nurses Association (ANA)
- Sigma Theta Tau International
- National League for Nursing (NLN)
- American Association of Colleges of Nursing (AACN)
Evidence-Based Practice Databases
- Cochrane Library
- PubMed/MEDLINE
- CINAHL
- Joanna Briggs Institute
Quality Improvement Resources
- Institute for Healthcare Improvement (IHI)
- Agency for Healthcare Research and Quality (AHRQ)
- The Joint Commission
- National Database of Nursing Quality Indicators (NDNQI)
Frequently Asked Questions: Evidence-Based Practice Nursing Topics 2025
Basic EBP Understanding
What is evidence-based practice in nursing?
Evidence-based practice (EBP) in nursing is a systematic approach that integrates three key components: the best available research evidence, clinical expertise, and patient values and preferences to make informed decisions about patient care. EBP ensures that nursing interventions are based on scientific research rather than tradition or personal opinion.
Why is evidence-based practice important for nursing students?
Evidence-based practice is crucial for nursing students because it:
- Improves patient outcomes by 15-20% according to healthcare studies
- Reduces medical errors and enhances patient safety
- Develops critical thinking and research skills
- Prepares students for professional nursing practice
- Meets accreditation requirements for nursing programs
- Builds confidence in clinical decision-making
What makes a good evidence-based practice topic?
A good EBP topic should be:
- Specific and focused – narrow enough to research thoroughly
- Clinically relevant – addresses current healthcare challenges
- Measurable – has clear outcomes that can be evaluated
- Feasible – can be completed within available time and resources
- Supported by evidence – has sufficient research literature available
- Impactful – can potentially improve patient care or nursing practice
Topic Selection and Research
What are the easiest EBP topics for nursing students?
The easiest EBP topics for beginners include:
- Hand hygiene compliance – observational study with clear metrics
- Patient fall prevention – specific protocol implementation
- Medication error reduction – double-checking procedures
- Patient education effectiveness – pre/post-test design
- Wound care protocols – standardized treatment comparison
- Pain assessment tools – tool effectiveness comparison
- Discharge planning – readmission rate analysis
What are the most popular EBP topics in 2025?
The most popular evidence-based practice topics for 2025 include:
- Digital health integration – telehealth, AI tools, mobile apps
- Mental health interventions – post-pandemic care, trauma-informed practice
- Infection control – antimicrobial resistance, hand hygiene protocols
- Geriatric care – fall prevention, dementia care, polypharmacy management
- Quality improvement – patient satisfaction, workflow optimization
- Technology adoption – electronic health records, clinical decision support
How do I choose an EBP topic for my specialty area?
To choose an EBP topic for your specialty:
- Identify current challenges in your practice area
- Review recent literature (2022-2025) in specialty journals
- Consider patient populations you work with most
- Assess available resources for research implementation
- Consult with clinical mentors for practical insights
- Align with career goals and personal interests
Research Process and Methodology
How long should an EBP project take?
Typical EBP project timelines:
- Undergraduate projects: 8-12 weeks
- Graduate projects: 12-16 weeks
- Doctoral projects: 6-12 months
Phase breakdown:
- Planning and literature review: 2-3 weeks
- Implementation: 4-8 weeks
- Data analysis and reporting: 2-3 weeks
What databases should I use for EBP research?
Essential databases for nursing EBP research:
- PubMed/MEDLINE – comprehensive medical literature
- CINAHL – nursing and allied health focus
- Cochrane Library – systematic reviews and meta-analyses
- Joanna Briggs Institute – evidence-based healthcare resources
- Google Scholar – broader academic search
- Ovid – medical and nursing databases
How many sources do I need for an EBP paper?
Source requirements by academic level:
- Undergraduate: 15-25 sources
- Graduate: 25-40 sources
- Doctoral: 40+ sources
Quality over quantity: Focus on peer-reviewed articles from the last 5 years, with emphasis on systematic reviews, meta-analyses, and randomized controlled trials.
Implementation and Evaluation
How do I implement an EBP project in a clinical setting?
Steps for clinical EBP implementation:
- Obtain permissions from facility administration
- Identify stakeholders and build support team
- Develop implementation plan with clear timelines
- Provide staff education on new protocols
- Pilot test with small group before full rollout
- Monitor progress and adjust as needed
- Evaluate outcomes using predetermined metrics
What are common barriers to EBP implementation?
Common EBP implementation barriers include:
- Time constraints – busy clinical schedules
- Resource limitations – funding, staffing, equipment
- Resistance to change – staff comfort with current practices
- Lack of research skills – difficulty interpreting evidence
- Organizational culture – limited support for innovation
- Technology challenges – system integration issues
How do I measure EBP project success?
Key success metrics for EBP projects:
- Patient outcomes – infection rates, readmissions, satisfaction scores
- Process improvements – workflow efficiency, error reduction
- Staff metrics – compliance rates, knowledge scores, satisfaction
- Cost-effectiveness – resource utilization, cost savings
- Quality indicators – safety measures, performance benchmarks
Specific Topic Areas
What are good EBP topics for medical-surgical nursing?
Top medical-surgical EBP topics:
- Wound care management – dressing protocols, healing optimization
- Post-operative care – early mobilization, pain management
- Medication safety – administration protocols, error prevention
- Patient education – discharge planning, self-care instructions
- Infection prevention – catheter care, surgical site infections
- Chronic disease management – diabetes care, heart failure protocols
What EBP topics work well for emergency nursing?
Emergency nursing EBP topics:
- Triage accuracy – protocol effectiveness, wait time reduction
- Sepsis recognition – early identification, treatment protocols
- Pain management – assessment tools, non-pharmacological interventions
- Trauma care – standardized protocols, team communication
- Mental health crises – de-escalation techniques, safety protocols
- Pediatric emergencies – age-appropriate care, family communication
What are trending EBP topics in critical care?
Critical care EBP trending topics:
- Delirium prevention – assessment tools, intervention strategies
- Ventilator weaning – protocol standardization, outcome improvement
- Family communication – ICU visitation, end-of-life discussions
- Pressure ulcer prevention – turning protocols, support surfaces
- Sedation management – light sedation protocols, daily interruption
- Infection control – VAP prevention, central line care
Academic Requirements
How do I format an EBP paper?
Standard EBP paper format:
- Title page – clear, descriptive title
- Abstract – 150-250 words summarizing key points
- Introduction – problem statement, significance
- Literature review – synthesis of current evidence
- Methodology – research design, data collection
- Results – findings presentation with statistics
- Discussion – interpretation, limitations, implications
- Conclusion – summary and recommendations
- References – APA format, peer-reviewed sources
What citation style should I use for EBP papers?
APA 7th edition is the standard citation style for nursing and healthcare research. Key requirements:
- In-text citations: (Author, Year)
- Reference list: alphabetical order
- DOI or URL for electronic sources
- Proper formatting for various source types
How do I write a PICOT question?
PICOT format for EBP questions:
- P – Patient/Population
- I – Intervention
- C – Comparison
- O – Outcome
- T – Time
Example: “In hospitalized elderly patients (P), does hourly rounding (I) compared to standard care (C) reduce fall rates (O) over a 30-day period (T)?”
Current Trends and Future Directions
What EBP topics address post-pandemic healthcare challenges?
Post-pandemic EBP focus areas:
- Telehealth effectiveness – remote monitoring, virtual consultations
- Infection control protocols – PPE optimization, visitor policies
- Mental health support – healthcare worker resilience, patient anxiety
- Workforce challenges – staffing models, burnout prevention
- Technology integration – contactless care, AI-assisted diagnosis
How is AI impacting EBP nursing topics?
AI’s impact on nursing EBP:
- Clinical decision support – diagnostic assistance, treatment recommendations
- Predictive analytics – risk assessment, early warning systems
- Workflow optimization – scheduling, resource allocation
- Patient monitoring – continuous assessment, alert systems
- Research synthesis – literature review, evidence mapping
What are emerging EBP topics for 2025?
Emerging 2025 EBP topics:
- Precision medicine – personalized care protocols
- Sustainability – green healthcare initiatives
- Health equity – addressing disparities, cultural competency
- Genomics integration – genetic testing, targeted therapies
- Virtual reality – pain management, therapeutic applications
- Wearable technology – continuous monitoring, self-care support
Practical Tips and Resources
Where can I find current EBP research?
Best sources for current EBP research:
- Professional journals – specialty nursing publications
- Professional organizations – ANA, AACN, specialty societies
- Government resources – AHRQ, CDC, NIH
- International sources – WHO, Cochrane Collaboration
- Academic institutions – university research centers
- Healthcare systems – quality improvement publications
How do I stay current with EBP trends?
Strategies for staying current:
- Subscribe to journals – nursing specialty publications
- Join professional organizations – networking and resources
- Attend conferences – latest research presentations
- Follow researchers – social media, academic profiles
- Set up alerts – database notifications for new research
- Participate in committees – institutional EBP initiatives
What resources are available for EBP support?
EBP support resources:
- Librarians – database searching, citation assistance
- Faculty mentors – research guidance, methodology support
- Clinical preceptors – practical implementation insights
- Writing centers – paper structure, formatting help
- Statistical consultants – data analysis support
- IRB committees – ethical review, approval processes
Common Mistakes and How to Avoid Them
What are common EBP mistakes nursing students make?
Common mistakes include:
- Too broad topics – narrow focus for better research
- Outdated sources – use recent literature (within 5 years)
- Weak PICOT questions – ensure specific, measurable outcomes
- Poor methodology – match design to research question
- Inadequate sample size – ensure sufficient participants
- Bias in analysis – maintain objectivity in interpretation
How do I avoid plagiarism in EBP papers?
Plagiarism prevention strategies:
- Proper citations – acknowledge all sources
- Paraphrasing – rewrite in your own words
- Quotation marks – for direct quotes
- Reference management – use tools like Zotero, EndNote
- Originality checks – use plagiarism detection software
- Understanding policies – know institutional requirements
This comprehensive FAQ section addresses the most common questions nursing students have about evidence-based practice topics, providing clear, actionable answers optimized for AI overview snippets and search engine visibility.

I am a professional nursing assignment expert offering comprehensive academic support to university nursing students across various institutions. My services are designed to help learners manage their workload effectively while maintaining academic excellence. With years of experience in nursing research, case study writing, and evidence-based reporting, I ensure every paper is original, well-researched, and aligned with current academic standards.
My goal is to provide dependable academic assistance that enables students to focus on practical training and career growth.
Contact me today to receive expert guidance and timely, high-quality nursing assignment help tailored to your academic needs.


