MS is a 35 year-old female with newly diagnosed depression. You have started discussing
Neurotransmitters and Mental Illness
MS is a 35 year-old female with newly diagnosed depression. You have started discussing initiating medication with her. She is a 4th-grade science teacher and asking you a lot of questions about what this means is happening in her brain. How would you explain to this patient how neurotransmitters work? Including, specifically how they affect mental illness. Which specific neurotransmitters would you address with her as they relate to her depression?
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Use Coupon Code: NEW30 to Get 30% OFF Your First Order
What is the Best Treatment Protocol for Major Depressive Disorder and Schizophrenia?
Major Depressive Disorder, commonly known as depression, is a mental health condition characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities.
Schizophrenia: Schizophrenia is a severe mental disorder that affects a person’s thoughts, emotions, and behaviors. Individuals with schizophrenia often experience disruptions in thinking, including hallucinations (perceiving things that are not present) and delusions (strongly held false beliefs). Other symptoms may include disorganized speech, impaired social functioning, reduced emotional expression, and cognitive deficits.
Schizophrenia typically emerges in late adolescence or early adulthood, and its exact cause is not fully understood, but it is believed to involve a combination of genetic, biological, and environmental factors. Treatment for schizophrenia often involves antipsychotic medications, psychotherapy, and support from mental health professionals and family members.
Impact of Major Depressive Disorder (MDD)
The impact of Major Depressive Disorder (MDD) and Schizophrenia on individuals and society is significant, affecting various aspects of a person’s life as well as the broader community. Here are some key considerations for both disorders:
- Individual Impact:
- Quality of Life: MDD can severely diminish the quality of life for individuals, impacting their ability to experience joy, engage in relationships, and pursue personal and professional goals.
- Physical Health: Depression is often associated with physical health issues such as changes in appetite, sleep disturbances, and a weakened immune system.
- Suicide Risk: Individuals with MDD may be at an increased risk of suicidal thoughts and behaviors, emphasizing the urgent need for proper intervention and support.
- Social Impact:
- Interpersonal Relationships: Depression can strain relationships with family, friends, and colleagues due to changes in mood, energy levels, and overall engagement.
- Workplace Productivity: MDD can lead to difficulties in concentration, decision-making, and overall workplace productivity, contributing to absenteeism and reduced performance.
- Economic Impact:
- Healthcare Costs: Treating and managing MDD requires significant healthcare resources, contributing to the economic burden on individuals, families, and society.
Impact of Schizophrenia:
- Individual Impact:
- Functional Impairment: Schizophrenia can lead to significant functional impairment, affecting a person’s ability to work, maintain relationships, and perform daily tasks.
- Stigma and Isolation: Individuals with schizophrenia may face social stigma, discrimination, and isolation due to the misperceptions and misconceptions surrounding the disorder.
- Social Impact:
- Family Dynamics: Families of individuals with schizophrenia may experience challenges in providing support and understanding, impacting family dynamics and relationships.
- Community Inclusion: Stigma related to schizophrenia can limit social inclusion and community participation, contributing to the isolation of affected individuals.
- Economic Impact:
- Treatment Costs: The economic burden of schizophrenia includes not only direct healthcare costs but also indirect costs related to lost productivity, unemployment, and the need for long-term care and support.
The Importance of Effective Treatment Protocols
The importance of effective treatment protocols for Major Depressive Disorder (MDD) cannot be overstated, as MDD is a serious and prevalent mental health condition that significantly impacts the well-being of affected individuals. Here are key reasons highlighting the importance of effective treatment protocols:
- Alleviating Individual Suffering:
- Effective treatment protocols aim to alleviate the intense emotional and psychological suffering experienced by individuals with MDD. Prompt and appropriate interventions can help reduce symptoms, improving overall quality of life.
- Reducing Suicide Risk:
- MDD is associated with an increased risk of suicidal thoughts and behaviors. Timely and effective treatment can mitigate this risk, providing essential support and intervention to individuals in crisis.
- Improving Daily Functioning:
- MDD often impairs daily functioning, affecting work, relationships, and overall productivity. Treatment protocols, including psychotherapy and medications, target symptoms to enhance cognitive and emotional functioning.
- Preventing Chronicity:
- Without proper treatment, MDD can become a chronic condition, leading to recurrent episodes and long-term impairment. Effective treatment protocols aim to prevent the progression to chronicity, promoting recovery and resilience.
- Enhancing Treatment Adherence:
- Well-structured treatment plans, tailored to individual needs, can enhance treatment adherence. Engaging individuals in a collaborative and supportive treatment process increases the likelihood of positive outcomes.
- Addressing Co-occurring Conditions:
- Individuals with MDD often experience co-occurring conditions, such as anxiety disorders or substance abuse. Comprehensive treatment protocols address these coexisting issues, promoting holistic well-being.
- Promoting Long-Term Stability:
- The goal of effective treatment is not only to alleviate acute symptoms but also to promote long-term stability. This involves developing coping mechanisms, resilience, and strategies for managing potential future challenges.
- Reducing Economic Burden:
- Untreated MDD can contribute to significant economic burdens through increased healthcare costs, workplace absenteeism, and reduced productivity. Effective treatment can mitigate these economic impacts by supporting individuals in maintaining or regaining their functional capacity.
- Enhancing Public Health:
- Successful treatment of MDD contributes to overall public health by reducing the prevalence and severity of mental health conditions. This, in turn, fosters a healthier and more productive society.
- Improving Relationships:
- MDD can strain interpersonal relationships. Effective treatment not only benefits the individual but also positively influences their relationships with family, friends, and colleagues.
Understanding Major Depressive Disorder (MDD)
Diagnostic Criteria for MDD
The diagnosis of Major Depressive Disorder (MDD) is typically made based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is a widely used manual for classifying mental health conditions. To be diagnosed with MDD, an individual must exhibit a certain number and combination of symptoms over a defined period. Here are the diagnostic criteria for Major Depressive Disorder:
- Depressed Mood or Loss of Interest:
- The presence of a depressed mood most of the day, nearly every day, as indicated by subjective reports or observations by others.
- A markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
- Additional Symptoms:
- Significant weight loss or weight gain, or a decrease or increase in appetite.
- Insomnia or hypersomnia nearly every day.
- Psychomotor agitation or retardation observable by others.
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive or inappropriate guilt.
- Diminished ability to think or concentrate, or indecisiveness.
- Recurrent thoughts of death, suicidal ideation without a specific plan, or a suicide attempt, or a specific plan for committing suicide.
- Duration and Functional Impairment:
- The symptoms must be present nearly every day for at least two weeks.
- The symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- Exclusion of Other Conditions:
- The symptoms are not due to the effects of a substance (e.g., drug abuse, medication) or another medical condition.
- No Manic or Hypomanic Episodes:
- The episode is not attributable to the physiological effects of a substance or another medical condition.
- The occurrence of a manic or hypomanic episode would suggest a diagnosis of Bipolar Disorder rather than MDD.
Prevalence and Global Impact of MDD
Prevalence of MDD:
- Global Prevalence: Major Depressive Disorder is a highly prevalent mental health condition worldwide. According to the World Health Organization (WHO), more than 264 million people of all ages suffer from depression globally.
- Lifetime Prevalence Rates: The lifetime prevalence of MDD varies across different populations. In the United States, for example, the National Institute of Mental Health (NIMH) reported that, as of 2019, approximately 20.6 million adults (or 8.4% of the U.S. population) had at least one major depressive episode in the past year.
- Gender Differences: Depression tends to be more common in women than in men. The NIMH reported that in 2019, the prevalence of MDD was higher among adult women (10.5%) compared to adult men (6.2%) in the United States.
Global Impact of MDD:
- Economic Burden: Major Depressive Disorder imposes a significant economic burden on individuals and societies. The costs associated with healthcare, lost productivity at work, and disability contribute to the economic impact.
- Disability and Impaired Functioning: MDD is a leading cause of disability worldwide. The condition can result in impaired social and occupational functioning, affecting an individual’s ability to carry out daily activities and maintain employment.
- Suicidal Ideation and Mortality: Depression is a major risk factor for suicide. Individuals with MDD are at an increased risk of suicidal ideation and attempts, emphasizing the importance of timely and effective intervention.
- Impact on Physical Health: Depression is associated with various physical health issues, including cardiovascular diseases, diabetes, and other chronic conditions. The interplay between mental and physical health underscores the comprehensive impact of MDD.
Risk Factors Associated with MDD
- Biological Factors:
- Genetics: A family history of depression increases the likelihood of developing MDD. Research suggests a genetic predisposition to the disorder.
- Brain Structure and Function: Alterations in the structure and function of certain brain regions, as observed through neuroimaging studies, may be associated with MDD.
- Psychological Factors:
- Personality Traits: Certain personality traits, such as high levels of neuroticism, may contribute to an increased vulnerability to depression.
- Cognitive Patterns: Negative thought patterns, such as persistent pessimism, self-criticism, and distorted thinking, are associated with an increased risk of MDD.
- Environmental Factors:
- Early Life Experiences: Adverse childhood experiences, trauma, or abuse can elevate the risk of developing depression later in life.
- Stressful Life Events: Significant life stressors, such as loss of a loved one, relationship difficulties, or financial problems, can trigger the onset of MDD.
- Medical Conditions:
- Chronic Illness: Certain medical conditions, such as chronic pain, diabetes, or cardiovascular diseases, may increase the risk of depression.
- Neurological Conditions: Some neurological disorders are associated with a higher prevalence of depressive symptoms.
- Medication and Substance Use:
- Medication: Certain medications, such as certain steroids or hormonal therapies, may contribute to the development of depression as a side effect.
- Substance Abuse: Substance abuse, including alcohol and drug misuse, is linked to an increased risk of MDD.
- Social Factors:
- Isolation and Lack of Social Support: Social isolation and a lack of supportive social connections are risk factors for depression.
- Socioeconomic Factors: Low socioeconomic status and limited access to resources may contribute to an elevated risk of MDD.
- Gender and Age:
- Gender: Women tend to be diagnosed with depression more frequently than men.
- Age: The risk of depression can vary across the lifespan, with certain age groups, such as adolescents and the elderly, being more susceptible.
Understanding Schizophrenia
Diagnostic Criteria for Schizophrenia
The diagnosis of Schizophrenia is based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is widely used for classifying mental health conditions. To be diagnosed with Schizophrenia, an individual must exhibit a combination of characteristic symptoms over a specific duration. Here are the diagnostic criteria for Schizophrenia according to the DSM-5:
A. Characteristic Symptoms:
- Delusions: False beliefs that are firmly held despite evidence to the contrary. Delusions are often bizarre or implausible.
- Hallucinations: Perceptions without external stimuli, such as hearing voices or seeing things that others do not.
- Disorganized Thinking (Speech): Disorganized thinking is typically manifested in disorganized or incoherent speech. This can include frequent derailment or incoherence.
- Grossly Disorganized or Abnormal Motor Behavior: This may manifest as unpredictable or inappropriate agitation, unpredictable movements, or a lack of movement altogether (catatonia).
- Negative Symptoms: Affective flattening (reduced emotional expression), alogia (poverty of speech), and anhedonia (reduced ability to experience pleasure).
B. Duration:
- Continuous signs of disturbance persist for at least six months. This must include at least one month of symptoms that meet Criterion A (active-phase symptoms).
C. Social/Occupational Dysfunction:
- The disturbance significantly impairs social, occupational, or other important areas of functioning.
D. Exclusion of Other Conditions:
- The symptoms are not attributable to another medical condition, substance use, or medication.
E. Schizoaffective and Mood Disorder Exclusion:
- Schizoaffective disorder and mood disorder with psychotic features have been ruled out, as the psychotic symptoms are not solely attributable to mood episodes.
F. Substance/General Medical Condition Exclusion:
- The disturbance is not due to the direct physiological effects of a substance (e.g., drugs, medications) or a general medical condition.
To meet the criteria for Schizophrenia, a specified number of characteristic symptoms must be present, and these symptoms must cause significant distress or impairment in social, occupational, or other important areas of functioning. The diagnosis should be made by a qualified mental health professional based on a comprehensive clinical assessment, considering the individual’s history and current symptoms.
Different Types of Schizophrenia
Schizophrenia is a complex mental health disorder, and while there isn’t a formal classification system for different types of schizophrenia in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), clinicians may describe various subtypes or presentations based on symptom patterns. Here are some terms commonly used to describe different types or subtypes of schizophrenia:
- Paranoid Schizophrenia:
- Characterized by prominent delusions and hallucinations. Individuals with paranoid schizophrenia often have irrational suspicions or beliefs that others are plotting against them.

- Characterized by prominent delusions and hallucinations. Individuals with paranoid schizophrenia often have irrational suspicions or beliefs that others are plotting against them.
- Disorganized Schizophrenia:
- Marked by disorganized thinking and speech. Individuals may have difficulty organizing their thoughts, making their speech incoherent or difficult to follow.
- Catatonic Schizophrenia:
- Features disturbances in movement. This can range from immobility and a lack of responsiveness (catatonic stupor) to excessive, purposeless movement (catatonic excitement).
- Residual Schizophrenia:
- Describes individuals who have had at least one episode of schizophrenia but are currently in a less severe phase. Residual symptoms may include mild hallucinations or withdrawal from social activities.
- Undifferentiated Schizophrenia:
- Used when a person does not clearly fit into one of the specific subtypes mentioned above. It may be applied when symptoms are varied and do not distinctly align with the criteria for a specific subtype.
- Schizoaffective Disorder:
- While not a subtype of schizophrenia, schizoaffective disorder shares features of schizophrenia and mood disorders. Individuals experience psychotic symptoms alongside mood disturbances, such as major depressive or manic episodes.
It’s important to note that these descriptors are used to capture the diversity of symptoms seen in individuals with schizophrenia. Additionally, the DSM-5 moved away from subtyping schizophrenia and instead emphasizes the dimensional assessment of symptoms and severity.
Individuals with schizophrenia can experience a range of symptoms, and the presentation may evolve over time. Treatment plans are often tailored to address the specific symptoms and needs of each person, and a comprehensive approach involving medication, psychotherapy, and support services is typically recommended. Diagnosis and treatment decisions should be made by qualified mental health professionals based on a thorough clinical assessment.
The Social and Economic Burden of Schizophrenia
Schizophrenia imposes a significant social and economic burden on individuals, families, and societies. The impact is multifaceted, affecting various aspects of life and contributing to both direct and indirect costs. Here are key points regarding the social and economic burden of schizophrenia:
Social Burden:
- Stigma and Discrimination:
- Individuals with schizophrenia often face stigma and discrimination, leading to social isolation and difficulty in forming and maintaining relationships. This can exacerbate the challenges they already face.
- Impaired Social Functioning:
- Schizophrenia can lead to impaired social functioning, making it difficult for individuals to engage in social activities, maintain friendships, or hold down jobs. This can contribute to a sense of isolation and exclusion.
- Impact on Families:
- Families of individuals with schizophrenia may experience strain and disruption. Providing care and support can be emotionally and physically demanding, affecting the overall well-being of family members.
- Educational and Occupational Challenges:
- Schizophrenia often manifests in early adulthood, impacting educational and occupational trajectories. Academic and vocational achievements may be compromised, affecting long-term life opportunities.
- Risk of Homelessness:
- Individuals with schizophrenia are at an increased risk of homelessness. The challenges in maintaining stable housing can exacerbate the overall social burden.
Economic Burden:
- Healthcare Costs:
- Treatment and management of schizophrenia involve significant healthcare costs. This includes expenses related to hospitalization, medication, therapy, and outpatient care.
- Lost Productivity:
- Schizophrenia can lead to substantial losses in productivity. Individuals may struggle to maintain employment or may be unable to work, contributing to both personal and societal economic losses.
- Unemployment and Underemployment:
- High levels of unemployment and underemployment are common among individuals with schizophrenia. This results in diminished personal income and increased dependence on social support programs.
- Criminal Justice System Costs:
- Some individuals with schizophrenia may come into contact with the criminal justice system, leading to additional economic burdens related to legal proceedings, incarceration, and associated services.
- Social Support Programs:
- Governments and communities often bear the economic burden of providing social support programs for individuals with schizophrenia. This includes disability benefits, housing assistance, and other forms of financial aid.
- Educational Costs:
- Educational challenges associated with schizophrenia may lead to increased costs for special education services and interventions.
Traditional Approaches to Treatment
Pharmacotherapy, or the use of medications, is a common and effective approach in the treatment of Major Depressive Disorder (MDD) and Schizophrenia. Here’s an overview of the pharmacological treatments for each condition:
Pharmacotherapy for Major Depressive Disorder (MDD)
- Antidepressant Medications:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Examples include fluoxetine, sertraline, and escitalopram. SSRIs increase the availability of serotonin, a neurotransmitter associated with mood regulation.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Medications like venlafaxine and duloxetine target both serotonin and norepinephrine pathways.
- Tricyclic Antidepressants (TCAs): Older antidepressants like amitriptyline and nortriptyline. They affect multiple neurotransmitters.
- Monoamine Oxidase Inhibitors (MAOIs): Rarely used due to dietary restrictions and potential side effects, MAOIs include phenelzine and tranylcypromine.
- Atypical Antidepressants:
- Bupropion: It affects norepinephrine and dopamine and is often used when sexual side effects or weight gain are concerns with other antidepressants.
- Augmentation Strategies:
- Augmenting with Other Medications: In cases of treatment-resistant depression, other medications like lithium, atypical antipsychotics, or thyroid hormones may be added to enhance the effectiveness of antidepressants.
- Electroconvulsive Therapy (ECT):
- In severe cases or when other treatments are ineffective, electroconvulsive therapy may be considered.
Pharmacotherapy for Schizophrenia:
- Antipsychotic Medications:
- Typical Antipsychotics (First Generation): Examples include haloperidol and chlorpromazine. They primarily block dopamine receptors and may lead to extrapyramidal side effects.
- Atypical Antipsychotics (Second Generation): Examples include risperidone, olanzapine, quetiapine, aripiprazole, and clozapine. These medications also affect serotonin receptors and generally have a lower risk of extrapyramidal side effects.
- Long-Acting Injectable Antipsychotics:
- Some antipsychotic medications are available in long-acting injectable forms, enhancing medication adherence.
- Adjunctive Medications:
- Antidepressants: May be prescribed if depression symptoms coexist with schizophrenia.
- Mood Stabilizers: In cases where mood instability is present, medications like lithium or certain anticonvulsants may be used.
- Clozapine:
- Reserved for treatment-resistant cases due to its potential for serious side effects. It is effective in managing symptoms but requires careful monitoring of blood counts.
- Electroconvulsive Therapy (ECT):
- In some cases of schizophrenia, particularly when there is resistance to medication, ECT may be considered.
Psychotherapy as a Treatment Modality
Psychotherapy, also known as talk therapy or counseling, is an important and evidence-based treatment modality for Major Depressive Disorder (MDD). It involves conversations between a trained mental health professional and an individual or group and aims to explore and address emotional and behavioral challenges. Here are some common types of psychotherapy used in the treatment of MDD:
- Cognitive-Behavioral Therapy (CBT):
- CBT is a widely used and effective form of psychotherapy for MDD. It focuses on identifying and challenging negative thought patterns and behaviors that contribute to depression. Through CBT, individuals learn to develop healthier thought patterns and coping strategies.
- Interpersonal Therapy (IPT):
- IPT is a time-limited psychotherapy that targets interpersonal issues that may contribute to depressive symptoms. It helps individuals improve their communication skills, navigate relationships, and address life changes or losses.
- Psychodynamic Therapy:
- Psychodynamic therapy explores unconscious processes and unresolved conflicts that may contribute to depression. It aims to increase self-awareness and understanding of how past experiences may influence current emotions and behaviors.
- Mindfulness-Based Cognitive Therapy (MBCT):
- MBCT combines elements of CBT with mindfulness practices. It helps individuals become more aware of their thoughts and emotions, teaching them to observe these experiences without judgment. MBCT is particularly effective in preventing the recurrence of depressive episodes.
- Dialectical Behavior Therapy (DBT):
- Originally developed for individuals with borderline personality disorder, DBT incorporates elements of CBT and mindfulness to help individuals manage intense emotions and improve interpersonal effectiveness.
- Problem-Solving Therapy:
- This therapy focuses on developing practical problem-solving skills. It helps individuals identify specific problems, set realistic goals, and work through potential solutions.
- Supportive Therapy:
- Supportive therapy provides emotional support and encouragement. It may be used in conjunction with other therapies to create a safe space for individuals to express themselves and explore their feelings.
Key Aspects of Psychotherapy for MDD:
- Collaborative Relationship:
- A strong therapeutic alliance between the individual and the therapist is crucial for the success of psychotherapy.
- Skill-Building:
- Many forms of psychotherapy for MDD involve teaching individuals coping skills, problem-solving techniques, and strategies for managing stress.
- Exploration of Emotions:
- Psychotherapy often involves exploring and processing emotions related to past and present experiences, providing individuals with a deeper understanding of their feelings.
- Goal-Setting:
- Establishing and working towards realistic goals is a common component of psychotherapy, helping individuals regain a sense of control and purpose.
- Relapse Prevention:
- Some psychotherapies, such as MBCT, focus on preventing the recurrence of depressive episodes by teaching skills to manage negative thought patterns.
Psychotherapy can be used as a standalone treatment for mild to moderate depression or in combination with medication for more severe cases. The choice of psychotherapy type depends on individual preferences, the specific nature of depressive symptoms, and the therapeutic approach of the mental health professional. Overall, psychotherapy offers a valuable and holistic approach to managing and treating Major Depressive Disorder.
Electroconvulsive Therapy (ECT) and Its Role
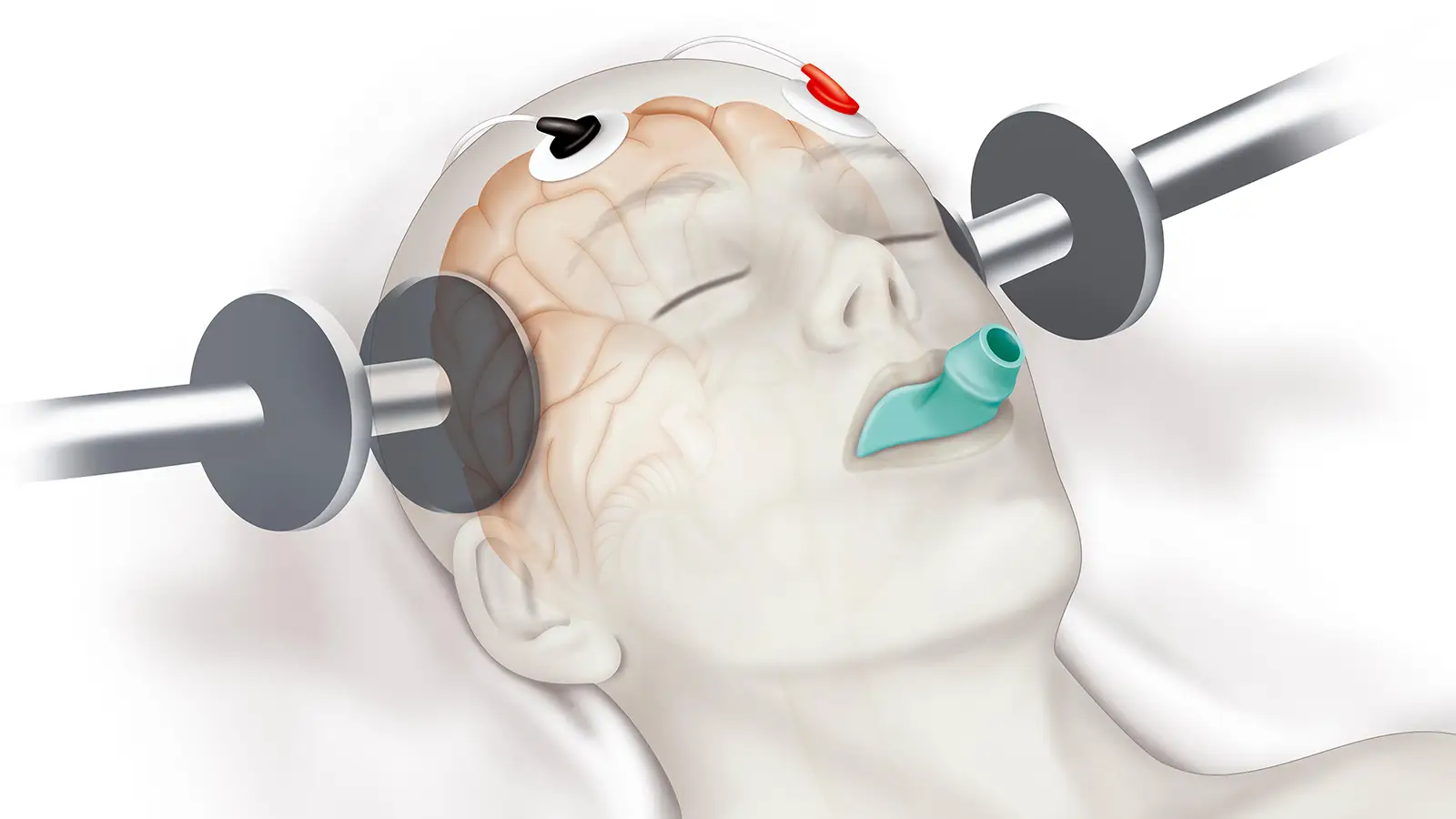
Electroconvulsive Therapy (ECT) is a medical treatment primarily used for severe mental health conditions, including Major Depressive Disorder (MDD) that has not responded to other forms of treatment. Here is an overview of ECT and its role in the treatment of MDD:
1. What is ECT?
- ECT involves the administration of a controlled electrical current to the brain, typically inducing a brief seizure. The procedure is conducted under general anesthesia and muscle relaxants to minimize discomfort and prevent injury during the seizure.
2. When is ECT Used for MDD?
- ECT is considered when MDD is severe, debilitating, and has not responded to other treatment modalities such as psychotherapy and medication. It may also be recommended in situations where rapid improvement is crucial, such as when an individual is at risk of harm due to severe depression.
3. Effectiveness:
- ECT has been shown to be highly effective, particularly in cases of severe and treatment-resistant depression. It often produces rapid and significant improvement in mood and other depressive symptoms.
4. Mechanism of Action:
- The exact mechanisms through which ECT works are not fully understood, but it is believed to induce changes in neurotransmitter activity in the brain. The therapeutic effects may involve alterations in the release and sensitivity of certain neurotransmitters.
5. Treatment Course:
- ECT is typically administered in a series of sessions, with the frequency and number of treatments determined by the individual’s response. A full course may consist of several treatments over a few weeks.
6. Side Effects:
- While ECT is generally considered safe, it can have side effects, including temporary memory loss and confusion immediately after treatment. However, these side effects tend to be short-term and gradually improve.
7. Patient Selection:
- The decision to use ECT is made collaboratively between the individual, their family, and the healthcare team. It is often recommended when other treatments have been ineffective or when a rapid response is necessary.
8. Maintenance ECT:
- Some individuals may benefit from ongoing or maintenance ECT sessions to prevent the recurrence of depressive symptoms. The frequency of maintenance treatments is tailored to the individual’s needs.
9. Modern ECT Techniques:
- Advances in ECT technology, including the use of brief-pulse stimuli and anesthesia, have reduced the risk of side effects and improved the overall safety and tolerability of the procedure.
10. Integration with Other Treatments:
- ECT may be used in conjunction with other treatments, such as psychotherapy and medication, to provide a comprehensive approach to managing severe depression.
Advancements in Neurostimulation Techniques
Transcranial Magnetic Stimulation (TMS) for MDD
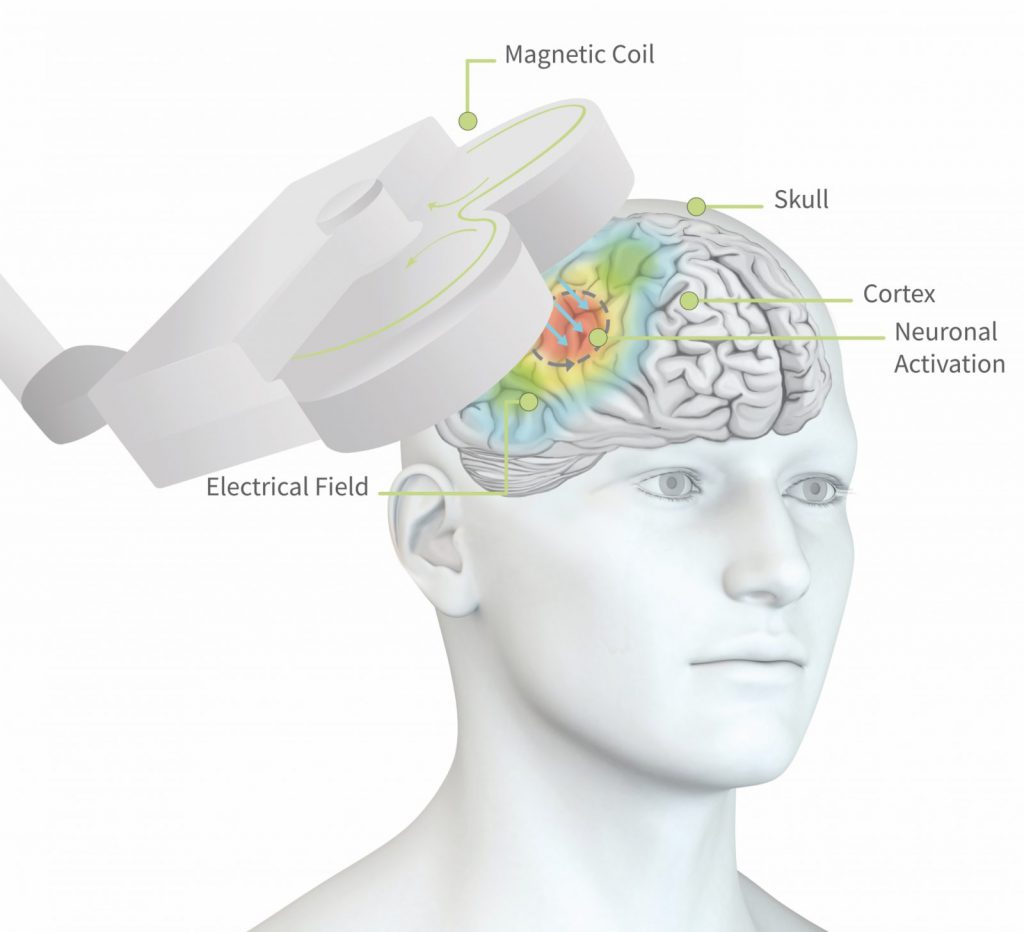
Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation technique that has been used as a treatment for Major Depressive Disorder (MDD), particularly for individuals who have not responded well to other forms of treatment. Here is an overview of TMS and its role in treating MDD:
1. What is TMS?
- TMS involves the use of a magnetic field to stimulate nerve cells in the brain. During a TMS session, an electromagnetic coil is placed against the scalp near the forehead, and magnetic pulses are delivered to stimulate targeted regions of the brain associated with mood regulation.
2. Mechanism of Action:
- The exact mechanism through which TMS works to alleviate depressive symptoms is not fully understood. It is believed to modulate neuronal activity in specific brain regions, leading to changes in neurotransmitter levels and improved mood regulation.
3. Treatment Course:
- TMS is typically administered as a series of sessions over several weeks. The frequency and duration of treatment sessions may vary depending on the specific protocol used and the individual’s response to the treatment.
4. Efficacy:
- TMS has been found to be effective in reducing depressive symptoms, and it is often considered for individuals with treatment-resistant depression. Research suggests that TMS may lead to improvements in mood, sleep, and overall functioning.
5. Non-Invasiveness:
- TMS is a non-invasive procedure that does not require anesthesia or sedation. Individuals undergoing TMS can resume their daily activities immediately after each session.
6. Side Effects:
- TMS is generally well-tolerated, and the side effects are usually mild and temporary. Common side effects may include scalp discomfort or headache during or after the treatment session.
7. Patient Selection:
- TMS is typically considered for individuals with MDD who have not responded adequately to antidepressant medications. It may also be a suitable option for those who cannot tolerate the side effects of medications.
8. Integration with Other Treatments:
- TMS can be used as a standalone treatment or in combination with other therapeutic modalities, such as psychotherapy and medication, to provide a comprehensive approach to managing depression.
9. Repetitive TMS (rTMS):
- Repetitive TMS (rTMS) involves the repeated delivery of magnetic pulses over time. High-frequency rTMS to the left dorsolateral prefrontal cortex is a common protocol used in the treatment of depression.
10. Maintenance TMS:
- Some individuals may benefit from maintenance TMS sessions to help prevent the recurrence of depressive symptoms after an initial course of treatment.
11. FDA Approval:
- TMS has received approval from the U.S. Food and Drug Administration (FDA) for the treatment of MDD in certain cases.
TMS is considered a promising and well-tolerated intervention for individuals with depression, especially when other treatments have not been effective. As with any medical intervention, it is essential for individuals considering TMS to discuss the potential risks, benefits, and suitability of the treatment with their healthcare provider.
Deep Brain Stimulation (DBS) in Schizophrenia Treatment
Deep Brain Stimulation (DBS) has not been established as a standard and widely accepted treatment for schizophrenia. DBS is a neurosurgical procedure that involves the implantation of electrodes into specific brain regions to modulate neural activity. While DBS has shown promise in the treatment of certain neurological and psychiatric conditions, its use in schizophrenia is still considered experimental, and research in this area is ongoing.
Here are key points regarding DBS in the context of schizophrenia:
- Research Status:
- Research investigating the potential effectiveness of DBS in schizophrenia is in the early stages. Clinical trials and studies are exploring the safety and efficacy of DBS in specific brain regions associated with the pathophysiology of schizophrenia.
- Targeted Brain Regions:
- Different studies have explored various brain targets for DBS in schizophrenia, including the ventral striatum and the anterior limb of the internal capsule. These regions are thought to be involved in the circuitry related to reward processing and emotional regulation, which are areas implicated in schizophrenia.
- Patient Selection:
- DBS for schizophrenia is not a standard treatment, and its use is generally considered in cases of treatment-resistant schizophrenia where individuals have not responded to other forms of therapy, including medications and psychotherapy.
- Potential Mechanisms:
- The precise mechanisms through which DBS may influence symptoms of schizophrenia are not fully understood. The modulatory effects of DBS on neural circuits and neurotransmitter systems are areas of interest in ongoing research.
- Ethical and Safety Considerations:
- DBS is an invasive procedure with potential risks, and ethical considerations surrounding its use in psychiatric disorders, including schizophrenia, are important. The long-term safety and ethical implications of using DBS for schizophrenia are subjects of ongoing debate and scrutiny.
- Individual Variability:
- Responses to DBS can vary among individuals, and researchers are working to identify patient characteristics that may predict positive outcomes. Factors such as the specific brain region targeted and individual variability in symptomatology may influence treatment response.
Vagus Nerve Stimulation (VNS) and Its Efficacy
Vagus Nerve Stimulation (VNS) is a neuromodulation technique that involves the implantation of a device that stimulates the vagus nerve, a major nerve that runs from the brain to various organs in the body. VNS has been approved by the U.S. Food and Drug Administration (FDA) for the treatment of certain medical conditions, including epilepsy and treatment-resistant depression. Here’s an overview of VNS and its efficacy, particularly in the context of depression:
1. How VNS Works:
- The VNS device is typically implanted under the skin on the chest, and a wire is threaded to the left vagus nerve. The device delivers electrical impulses to the vagus nerve, and these impulses are then transmitted to various areas of the brain.
2. FDA Approval for Depression:
- VNS has received FDA approval as an adjunctive (additional) treatment for chronic or recurrent treatment-resistant depression in individuals 18 years and older. It is meant to be used in conjunction with standard antidepressant medications.
3. Mechanism of Action:
- The exact mechanisms through which VNS exerts its antidepressant effects are not fully understood. It is believed to modulate neural circuits and neurotransmitter systems involved in mood regulation, including serotonin and norepinephrine pathways.
4. Efficacy in Depression:
- Clinical studies and research suggest that VNS can be effective in reducing symptoms of depression, particularly in individuals who have not responded well to multiple antidepressant medications. The improvement in symptoms may take several weeks to months.
5. Treatment Course:
- VNS is a long-term treatment, and its benefits may become more apparent over time. The device is programmed by healthcare professionals to deliver specific patterns of stimulation.
6. Safety and Side Effects:
- VNS is generally considered safe, and side effects are often mild and transient. Common side effects may include voice changes, cough, and neck pain. Serious side effects are rare but can include hoarseness or difficulty swallowing.
7. Patient Selection:
- VNS is typically considered for individuals with chronic or recurrent depression who have not responded to multiple antidepressant treatments. The decision to use VNS is made collaboratively between the individual and their healthcare team.
8. Research and Ongoing Studies:
- Ongoing research is exploring the efficacy of VNS in various psychiatric and neurological conditions. This includes studies on its potential use in bipolar disorder, anxiety disorders, and other neuropsychiatric conditions.
9. Individual Response:
- Responses to VNS can vary among individuals, and its efficacy may depend on factors such as the duration and severity of depression, the presence of comorbid conditions, and individual variability in treatment response.
While VNS can be a valuable option for some individuals with treatment-resistant depression, it is important to note that it is not a first-line treatment, and its use is typically reserved for specific cases. Individuals considering VNS should undergo a thorough evaluation by mental health professionals to determine its suitability for their specific situation.
Emerging Trends in Psychiatric Medications
Ketamine and Esketamine for Treatment-Resistant Depression
Ketamine and its derivative esketamine have gained attention in recent years for their potential as rapid-acting antidepressants, particularly in the treatment of individuals with treatment-resistant depression (TRD). Here’s an overview of ketamine and esketamine in the context of depression:
1. Ketamine:
- Mechanism of Action: Ketamine is an anesthetic agent that, at subanesthetic doses, has been found to modulate glutamate neurotransmission. The exact mechanisms underlying its antidepressant effects are still being studied.
- Administration: Ketamine is often administered intravenously (IV), intramuscularly (IM), or orally. The intravenous route is commonly used for its rapid onset of action.
- Efficacy: Clinical studies have shown that ketamine can produce rapid and significant antidepressant effects, often within hours or days. However, the effects are typically not long-lasting, and maintenance treatments may be necessary.
- Treatment Setting: Ketamine is often administered in a controlled clinical setting under the supervision of healthcare professionals.
2. Esketamine:
- Derivative of Ketamine: Esketamine is the S-enantiomer of ketamine. It is the active ingredient in the intranasal medication known as Spravato.
- FDA Approval: Esketamine nasal spray received FDA approval for the treatment of TRD in adults in conjunction with an oral antidepressant. It is specifically indicated for individuals who have not responded adequately to at least two different antidepressant treatments.
- Administration: Esketamine is self-administered under the supervision of a healthcare professional. The typical dosing schedule involves twice-weekly administration during the initial weeks, followed by a reduction to once-weekly or every other week.
- Monitoring: Due to potential side effects, individuals receiving esketamine are monitored for at least two hours post-administration.
3. Rapid Onset of Action:
- Both ketamine and esketamine are known for their rapid onset of antidepressant effects, which is in contrast to traditional antidepressants that may take weeks to show efficacy.
4. Safety Considerations:
- While ketamine and esketamine can be effective, their safety profiles are still being studied. They may be associated with side effects such as dissociation, increases in blood pressure, and sedation.
5. Individual Response:
- Response to ketamine and esketamine can vary among individuals. Some individuals may experience a significant and sustained reduction in depressive symptoms, while others may not respond as effectively.
6. Maintenance Treatment:
- For many individuals, the antidepressant effects of ketamine and esketamine are not long-lasting. Maintenance treatments may be necessary to sustain the benefits over time.
7. Ongoing Research:
- Research is ongoing to further understand the long-term efficacy and safety of ketamine and esketamine. Additionally, investigations are exploring their potential role in other psychiatric conditions.

Cannabinoids in the Management of Psychiatric Disorders
Cannabinoids, the active compounds found in the cannabis plant, have been of increasing interest in the field of psychiatry for their potential therapeutic effects on various mental health conditions. Here’s an overview of cannabinoids in the management of psychiatric disorders:
1. Cannabinoids and the Endocannabinoid System:
- The endocannabinoid system (ECS) is a complex cell-signaling system that plays a role in regulating a range of physiological processes, including mood, stress, and sleep. Cannabinoids, both endogenous (produced within the body) and exogenous (found in cannabis), interact with the ECS.
2. Cannabidiol (CBD) and Psychiatric Disorders:
- Anxiety Disorders: CBD has been studied for its potential anxiolytic (anxiety-reducing) effects. Some research suggests that it may be beneficial for conditions such as generalized anxiety disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD).
- Depressive Disorders: Limited research indicates that CBD may have antidepressant-like effects, potentially by influencing serotonin receptors in the brain. However, more research is needed to establish its efficacy in treating depression.
- Psychotic Disorders: CBD has been explored for its antipsychotic properties and its potential to mitigate symptoms of psychosis. Research in this area includes investigations into its use in schizophrenia and related disorders.
3. Tetrahydrocannabinol (THC) and Psychiatric Effects:
- Euphoria and Psychosis Risk: THC is the psychoactive component of cannabis responsible for the “high” sensation. While it may produce euphoria, high doses of THC can also induce anxiety and paranoia. In susceptible individuals, particularly those with a predisposition to psychosis, THC may increase the risk of psychotic episodes.
4. Cannabinoids in Post-Traumatic Stress Disorder (PTSD):
- Some studies have explored the potential use of cannabinoids, particularly CBD, in the treatment of PTSD. CBD’s effects on fear extinction and memory processes are areas of interest in this context.
5. Bipolar Disorder and Cannabinoids:
- Research on the use of cannabinoids in bipolar disorder is limited. The potential mood-stabilizing effects of cannabinoids are still under investigation.
6. Safety Considerations:
- While cannabinoids, particularly CBD, are generally considered safe, potential side effects and interactions with other medications should be considered. THC, in higher doses, can lead to impairments in cognitive function and coordination.
7. Regulatory Status:
- The legal status of cannabinoids varies globally and within different regions. Medical cannabis and cannabinoid-derived medications are subject to specific regulations and may be legally prescribed in some areas.
8. Individual Responses:
- Responses to cannabinoids can vary widely among individuals, and the optimal dosage and formulation may differ based on the specific psychiatric condition and individual characteristics.
9. Research Challenges:
- The field of cannabinoid research faces challenges, including the need for well-designed clinical trials, standardization of products, and a better understanding of the long-term effects of cannabinoid use.
Personalized Medicine and its Role in Psychiatric Treatment
Personalized medicine in psychiatry refers to the tailoring of medical treatment to the individual characteristics of each patient. This approach takes into account factors such as an individual’s genetic makeup, biomarkers, lifestyle, and environmental influences to optimize treatment outcomes. Here’s an overview of the role of personalized medicine in psychiatric treatment:
1. Genetic Factors:
- Pharmacogenomics: Examining an individual’s genetic profile can provide insights into how they metabolize and respond to medications. Pharmacogenomic testing can help identify genetic variations that may influence medication efficacy and potential side effects.
- Genetic Risk Factors: Genetic factors can contribute to an individual’s susceptibility to certain psychiatric disorders. Understanding these genetic risk factors may inform treatment strategies and risk assessment.
2. Biomarkers and Neuroimaging:
- Biomarkers: Identifying biomarkers associated with specific psychiatric disorders can aid in diagnosis and treatment planning. For example, blood tests or neuroimaging techniques may reveal markers indicative of a particular disorder or treatment response.
- Neuroimaging: Advanced imaging technologies, such as functional magnetic resonance imaging (fMRI) or positron emission tomography (PET), can provide insights into brain structure and function. This information may guide treatment decisions and help monitor treatment progress.
3. Targeted Medication Selection:
- Psychopharmacogenetics: By considering an individual’s genetic makeup, healthcare providers can make more informed decisions about which psychiatric medications are likely to be most effective and have fewer side effects for a particular patient.
- Trial-and-Error Reduction: Personalized medicine can help reduce the trial-and-error approach often seen in psychiatric medication management. This can lead to quicker and more effective treatment outcomes.
4. Treatment Response Prediction:
- Predictive Modeling: Integrating various factors, including genetic information, biomarkers, and clinical history, can help create predictive models for treatment response. This can guide clinicians in selecting interventions more likely to succeed for a specific individual.
5. Lifestyle and Environmental Factors:
- Individualized Treatment Plans: Personalized medicine acknowledges the importance of considering an individual’s lifestyle, environmental stressors, and social support systems when developing treatment plans. Lifestyle interventions, such as exercise and diet, can be tailored to the individual.
- Environmental Sensitivity: Some individuals may be more sensitive to environmental factors, such as trauma or stress. Personalized medicine takes into account these unique sensitivities when designing treatment strategies.
6. Patient Engagement and Shared Decision-Making:
- Informed Decision-Making: Personalized medicine emphasizes involving patients in the decision-making process. Informed patients can actively participate in selecting treatments that align with their preferences, values, and lifestyle.
- Continuous Monitoring: Personalized medicine supports ongoing monitoring of treatment effectiveness, allowing for adjustments based on a patient’s changing needs and responses.
7. Challenges and Future Directions:
- Data Integration: Integrating diverse sources of information, such as genetic data, biomarkers, and clinical history, poses challenges in terms of data interpretation and privacy concerns.
- Evidence Base: Establishing a robust evidence base for personalized medicine in psychiatry requires large-scale studies and collaborations across disciplines.
Integrative Approaches to Treatment
The Role of Nutrition in Mental Health
Nutrition plays a crucial role in mental health, influencing brain function, neurotransmitter production, and overall well-being. The relationship between diet and mental health is complex, involving various nutrients that contribute to cognitive function, mood regulation, and the prevention of mental health disorders. Here’s an overview of the role of nutrition in mental health:
1. Nutrients and Brain Function:
- Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, omega-3 fatty acids are essential for brain health. They contribute to the structure of brain cell membranes and play a role in neurotransmitter function.
- Vitamins and Minerals: Adequate intake of vitamins and minerals, including B vitamins (particularly B6, B9, and B12), vitamin D, zinc, and magnesium, is essential for neurotransmitter synthesis and overall brain function.
- Antioxidants: Fruits and vegetables rich in antioxidants, such as vitamins C and E, help protect the brain from oxidative stress. Oxidative stress has been linked to mental health disorders.
2. Gut-Brain Connection:
- Microbiome Health: The gut microbiome, the collection of microorganisms in the digestive system, influences mental health. A balanced and diverse microbiome is associated with better mood and cognitive function.
- Probiotics: Consuming probiotics, found in fermented foods like yogurt and kimchi, can support a healthy gut microbiome and may have positive effects on mental well-being.
3. Impact of Diet on Mood:
- Blood Sugar Regulation: Consuming a balanced diet with complex carbohydrates, fiber, and proteins helps regulate blood sugar levels. Stable blood sugar is crucial for mood stability and energy levels.
- Hydration: Dehydration can negatively impact mood and cognitive function. Maintaining adequate hydration is essential for overall well-being.
4. Influence on Mental Health Disorders:
- Depression and Anxiety: Some studies suggest a link between a nutrient-rich diet and a lower risk of depression and anxiety. Conversely, poor nutrition, particularly diets high in processed foods, has been associated with an increased risk of mental health disorders.
- Neurodegenerative Disorders: Certain nutrients, such as antioxidants and omega-3 fatty acids, may play a protective role against neurodegenerative disorders like Alzheimer’s disease.
5. Role of Macronutrients:
- Proteins: Amino acids from protein sources are essential for the synthesis of neurotransmitters like serotonin and dopamine, which impact mood.
- Carbohydrates: Complex carbohydrates, such as whole grains and vegetables, provide a steady supply of glucose to the brain, supporting cognitive function.
- Fats: Healthy fats, including monounsaturated and polyunsaturated fats, contribute to brain structure and function. Sources include avocados, olive oil, and nuts.
6. Individual Variability:
- Biochemical Individuality: Nutritional needs can vary among individuals based on factors such as genetics, metabolism, and overall health. Understanding individual nutritional needs is essential for personalized mental health support.
7. Nutritional Interventions:
- Dietary Approaches: Adopting a balanced and varied diet that includes a wide range of nutrient-dense foods is a fundamental approach to supporting mental health.
- Supplementation: In some cases, nutritional supplements may be recommended to address specific deficiencies or support mental well-being. However, it’s crucial to consult with a healthcare professional before starting any supplementation.
Exercise as a Complementary Treatment
Exercise is recognized as a valuable and complementary treatment for various mental health conditions. Engaging in regular physical activity has been shown to have positive effects on mood, cognition, and overall well-being. Here’s an overview of the role of exercise as a complementary treatment:
1. Mood Enhancement:
- Release of Endorphins: Exercise triggers the release of endorphins, neurotransmitters that act as natural mood lifters. This can contribute to an improved sense of well-being and a reduction in symptoms of anxiety and depression.
- Stress Reduction: Physical activity helps reduce levels of stress hormones, such as cortisol. Regular exercise can enhance the body’s ability to manage and cope with stressors.
2. Neurotransmitter Regulation:
- Serotonin and Dopamine: Exercise has been linked to increased production and release of neurotransmitters such as serotonin and dopamine. These play key roles in mood regulation and pleasure.
- Brain-Derived Neurotrophic Factor (BDNF): Exercise promotes the release of BDNF, a protein that supports the growth and maintenance of nerve cells. BDNF is associated with cognitive function and has implications for mental health.
3. Cognitive Benefits:
- Improved Cognitive Function: Regular physical activity is associated with improved cognitive function, including enhanced memory, attention, and executive function. This can be particularly relevant in conditions such as attention deficit hyperactivity disorder (ADHD) and cognitive decline associated with aging.
- Neuroprotective Effects: Exercise may have neuroprotective effects, helping to mitigate the risk of neurodegenerative disorders and supporting overall brain health.
4. Sleep Improvement:
- Regulation of Sleep Patterns: Exercise can contribute to the regulation of sleep patterns, promoting better sleep quality. Improved sleep is crucial for mental health and overall well-being.
5. Social Interaction:
- Social Engagement: Group exercise activities provide opportunities for social interaction, fostering a sense of community and support. Social engagement is important for mental health, especially in conditions where social withdrawal is a concern.
6. Complementary Treatment for Mental Health Disorders:
- Depression and Anxiety: Exercise has been shown to be effective as a complementary treatment for depression and anxiety. It may be used alone or in conjunction with other therapeutic interventions.
- Post-Traumatic Stress Disorder (PTSD): Physical activity has been explored as part of treatment plans for individuals with PTSD, offering benefits for both physical and mental well-being.
- Attention Deficit Hyperactivity Disorder (ADHD): Regular exercise has been associated with improvements in attention, impulse control, and hyperactivity in individuals with ADHD.
7. Duration and Intensity:
- Consistency is Key: The mental health benefits of exercise are often linked to consistency rather than intensity. Regular, moderate-intensity exercise is generally recommended for optimal well-being.
8. Types of Exercise:
- Aerobic Exercise: Activities such as walking, running, swimming, and cycling have been shown to have positive effects on mood and mental health.
- Strength Training: Resistance training can also contribute to mental health benefits, promoting a sense of accomplishment and physical well-being.
9. Individualized Approach:
- Personal Preferences: Choosing types of exercise that individuals enjoy increases the likelihood of adherence. Whether it’s dancing, hiking, or team sports, the key is to find activities that bring joy.
10. Consultation with Healthcare Professionals:
- Individualized Plans: Before starting an exercise regimen, especially for individuals with pre-existing health conditions, it’s important to consult with healthcare professionals to ensure that the chosen activities are safe and suitable.
Mind-Body Practices in MDD and Schizophrenia Management
Mind-body practices encompass a variety of techniques that integrate the mind and body to enhance health and well-being. While these practices are not standalone treatments for major depressive disorder (MDD) or schizophrenia, they can be valuable components of a comprehensive management plan. Here’s an overview of how mind-body practices can be incorporated into the management of MDD and schizophrenia:
1. Mindfulness Meditation:
- MDD: Mindfulness-based interventions, including mindfulness meditation, have shown promise in reducing symptoms of depression. Mindfulness involves cultivating non-judgmental awareness of the present moment, promoting emotional regulation and stress reduction.
- Schizophrenia: Mindfulness practices can complement traditional treatments for schizophrenia by helping individuals manage stress, improve focus, and enhance overall well-being.
2. Yoga:
- MDD: Yoga, with its combination of physical postures, breath control, and meditation, has been associated with improvements in depressive symptoms. It may enhance mood, reduce anxiety, and contribute to a sense of calm.
- Schizophrenia: While more research is needed, some studies suggest that yoga may have benefits for individuals with schizophrenia by improving cognitive functioning and reducing symptoms.
3. Tai Chi:
- MDD: Tai Chi, a gentle martial art characterized by slow, flowing movements, has demonstrated positive effects on mood and stress reduction. It may be particularly suitable for individuals with MDD who prefer low-impact activities.
- Schizophrenia: Tai Chi may help improve balance, coordination, and overall physical well-being in individuals with schizophrenia. It can be adapted to various fitness levels.
4. Breathing Exercises:
- MDD: Deep breathing exercises, such as diaphragmatic breathing or paced breathing, can activate the relaxation response, reducing physiological and psychological stress associated with depression.
- Schizophrenia: Breath-focused practices can be helpful in managing anxiety and improving concentration in individuals with schizophrenia. They are non-intrusive and can be easily incorporated into daily routines.
5. Progressive Muscle Relaxation (PMR):
- MDD: PMR, a technique involving the systematic tensing and relaxing of muscle groups, can be effective in reducing muscle tension and promoting relaxation, contributing to stress and anxiety reduction.
- Schizophrenia: PMR may help individuals with schizophrenia manage muscle tension and improve body awareness. It can be particularly useful in enhancing overall relaxation.
6. Biofeedback:
- MDD: Biofeedback, which involves monitoring physiological functions and providing feedback to help individuals gain control over their responses, can be used to manage stress and promote relaxation in individuals with MDD.
- Schizophrenia: While less studied, biofeedback may have potential applications in schizophrenia treatment by helping individuals develop better self-regulation skills.
7. Dance Movement Therapy:
- MDD: Dance movement therapy incorporates movement and expression to support emotional and physical well-being. It can be a creative and embodied approach to managing depressive symptoms.
- Schizophrenia: Dance movement therapy may be adapted to help individuals with schizophrenia improve body awareness, self-expression, and social interaction.
8. Art and Expressive Therapies:
- MDD: Art and expressive therapies, including visual arts, music, and drama therapy, can provide avenues for self-expression, emotional processing, and creative exploration in the context of depression.
- Schizophrenia: Creative and expressive therapies may contribute to social engagement, emotional expression, and cognitive functioning in individuals with schizophrenia.
9. Integration into Treatment Plans:
- Collaborative Approach: Mind-body practices are most effective when integrated into a collaborative and individualized treatment plan developed with mental health professionals. They should complement rather than replace standard treatments.
10. Safety and Suitability:
- Individual Considerations: Mind-body practices should be chosen based on individual preferences, physical health, and the severity of symptoms. It’s important to ensure that selected practices are safe and suitable for each individual’s unique circumstances.
Addressing Comorbidities
Managing Anxiety and Depression in Schizophrenia Patients
Managing anxiety and depression in individuals with schizophrenia poses unique challenges due to the complex interplay of symptoms and the potential impact on overall well-being. Here are strategies and considerations for addressing anxiety and depression in individuals with schizophrenia:
1. Comprehensive Assessment:
- Understand the Underlying Causes: Thoroughly assess the causes and contributing factors of anxiety and depression in individuals with schizophrenia. Consider biological, psychological, and social factors.
2. Medication Management:
- Antipsychotic Medications: Ensure that antipsychotic medications are effectively managing positive symptoms of schizophrenia. Adjustments to medication may be necessary to address both positive and negative symptoms.
- Adjunctive Medications: Depending on the severity of anxiety and depression, adjunctive medications such as antidepressants or anxiolytics may be considered. However, their use should be carefully monitored due to potential interactions with antipsychotic medications.
3. Psychoeducation:
- Educate the Individual and Caregivers: Provide education on the relationship between schizophrenia, anxiety, and depression. Enhance understanding of symptoms, treatment options, and the importance of adherence to medications.
4. Cognitive Behavioral Therapy (CBT):
- Targeted Interventions: CBT adapted for individuals with schizophrenia (CBT for psychosis) can be beneficial. It addresses distorted thinking patterns, reduces negative symptoms, and provides coping strategies for anxiety and depression.
5. Supportive Psychotherapy:
- Establishing Trust: Supportive psychotherapy can help build trust and rapport with individuals experiencing schizophrenia. A therapeutic relationship can provide a safe space for discussing emotions and addressing concerns.
6. Social Support:
- Engage with Support Systems: Encourage involvement in supportive social networks, including friends, family, or support groups. Social connections can provide emotional support and reduce feelings of isolation.
7. Lifestyle Modifications:
- Physical Activity: Encourage regular physical activity, as exercise has been shown to have positive effects on mood and can be a helpful adjunct to treatment.
- Healthy Diet: Promote a balanced and nutritious diet, as nutritional factors can influence mental health. Consult with a healthcare professional for dietary recommendations.
- Adequate Sleep: Ensure sufficient and regular sleep, as sleep disturbances can exacerbate symptoms of anxiety and depression.
8. Stress Management:
- Stress Reduction Techniques: Teach stress management techniques such as deep breathing, mindfulness, or progressive muscle relaxation. These techniques can help individuals cope with anxiety and reduce overall stress levels.
9. Monitoring and Regular Follow-ups:
- Regular Assessments: Conduct regular assessments of symptoms and treatment effectiveness. Monitor for side effects of medications and adjust treatment plans as needed.
10. Individualized Treatment Plans:
- Tailor Interventions: Recognize the individuality of each person with schizophrenia. Tailor treatment plans to address their specific needs, preferences, and strengths.
11. Addressing Co-occurring Substance Use:
- Substance Use Treatment: Address any co-occurring substance use issues, as substance use can worsen symptoms of anxiety and depression in individuals with schizophrenia.
12. Collaboration Between Providers:
- Multidisciplinary Approach: Foster collaboration between mental health professionals, including psychiatrists, psychologists, social workers, and other healthcare providers, to ensure a comprehensive and coordinated approach to treatment.
Addressing Cognitive Impairment in MDD Treatment
Cognitive impairment is a common aspect of Major Depressive Disorder (MDD) that can significantly impact daily functioning and quality of life. Addressing cognitive symptoms is an important component of MDD treatment. Here are strategies and considerations for managing cognitive impairment in the treatment of MDD:
1. Thorough Assessment:
- Identify Cognitive Symptoms: In the assessment of MDD, specifically evaluate cognitive symptoms such as difficulties with concentration, memory, decision-making, and executive function.
2. Medication Management:
- Antidepressant Selection: Choose antidepressant medications that not only target mood symptoms but also have a favorable impact on cognitive function. Some antidepressants may have cognitive-enhancing effects.
- Adjunctive Medications: Consider adjunctive medications or augmentation strategies if cognitive symptoms persist. These may include medications that address specific cognitive deficits, such as cognitive enhancers or stimulants.
3. Cognitive-Behavioral Therapy (CBT):
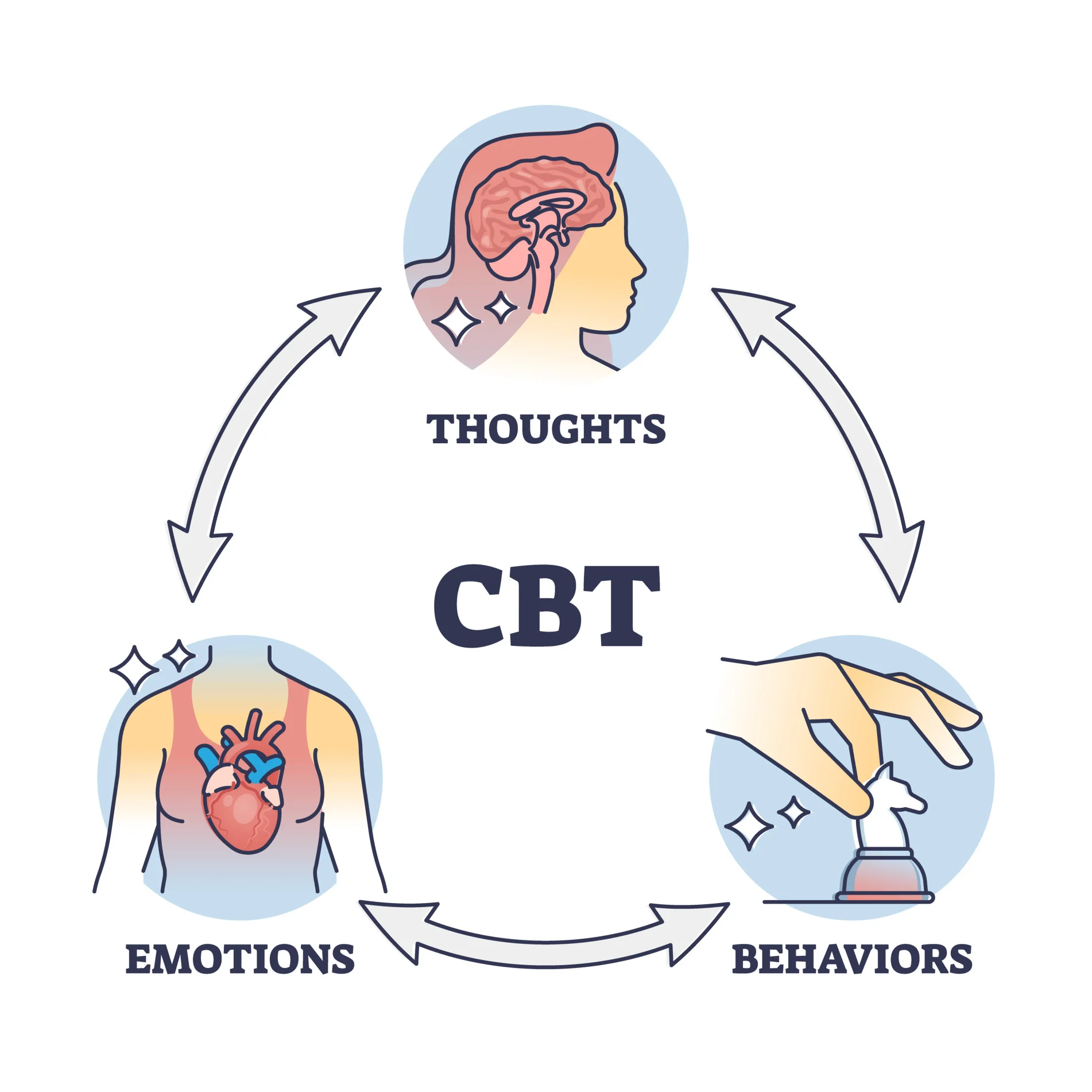
- Cognitive Remediation: Incorporate cognitive remediation strategies within CBT. This may involve techniques to challenge and reframe negative thought patterns, improve cognitive flexibility, and enhance problem-solving skills.
4. Psychoeducation:
- Educate Patients: Provide psychoeducation about the cognitive symptoms associated with MDD. Help patients understand that cognitive impairment is a recognized aspect of depression and that addressing mood symptoms can also positively impact cognitive function.
5. Lifestyle Interventions:
- Physical Exercise: Encourage regular physical exercise, as it has been shown to have positive effects on both mood and cognitive function. Exercise increases blood flow to the brain and promotes the release of neurotransmitters associated with cognitive well-being.
- Healthy Diet: Promote a balanced and nutritious diet, as nutritional factors can influence cognitive function. Certain dietary patterns, such as the Mediterranean diet, have been associated with cognitive benefits.
- Adequate Sleep: Ensure that patients are getting sufficient and restorative sleep. Sleep disturbances can contribute to cognitive impairment and addressing them can improve overall cognitive function.
6. Cognitive Training Programs:
- Computerized Cognitive Training: Consider computerized cognitive training programs that target specific cognitive domains. These programs may include exercises designed to enhance memory, attention, and executive function.
7. Address Co-occurring Conditions:
- Identify and Treat Comorbidities: Address and manage any comorbid conditions that may contribute to cognitive impairment, such as anxiety disorders or medical conditions.
8. Regular Follow-ups and Monitoring:
- Ongoing Assessment: Conduct regular follow-ups to monitor changes in cognitive symptoms over time. Adjust treatment plans based on the individual’s response and evolving needs.
9. Individualized Treatment Plans:
- Tailor Interventions: Recognize that cognitive impairment can vary among individuals with MDD. Tailor treatment plans to address specific cognitive deficits and take into account the unique needs and preferences of each patient.
10. Collaboration Between Providers:
- Multidisciplinary Approach: Foster collaboration between mental health professionals, including psychiatrists, psychologists, and other healthcare providers. A multidisciplinary approach can provide a comprehensive and coordinated strategy for addressing cognitive impairment.
11. Patient Engagement:
- Involve Patients in Treatment Planning: Engage patients in discussions about their cognitive symptoms and involve them in the development of strategies to address these challenges. Empowerment and active participation in treatment can enhance motivation and outcomes.
12. Manage Expectations:
- Realistic Expectations: Set realistic expectations for the improvement of cognitive symptoms. Improvement may be gradual and may require a combination of interventions.
The Interplay of Substance Use Disorders
The interplay of substance use disorders (SUDs) and major depressive disorder (MDD) can be complex and challenging to address due to the bidirectional influence of these conditions. Comorbidities of SUDs and MDD often present overlapping symptoms and shared risk factors. Here’s an overview of the interplay and considerations for addressing comorbidities in MDD:
1. Shared Risk Factors:
- Biological Vulnerability: Genetic factors may contribute to an increased risk for both substance use disorders and major depressive disorder. Individuals with a family history of either condition may be more susceptible to developing comorbidities.
- Neurobiological Changes: Both MDD and substance use can affect the brain’s reward system and neurotransmitter pathways, contributing to the development and maintenance of comorbid conditions.
2. Self-Medication and Coping:
- Coping Mechanism: Individuals with MDD may use substances as a way to cope with the symptoms of depression. The temporary relief provided by substances can lead to a cycle of self-medication.
- Increased Vulnerability: Substance use, especially in the context of self-medication, can exacerbate depressive symptoms and contribute to a worsening of MDD.
3. Dual Diagnosis and Treatment Challenges:
- Complex Presentation: Comorbidities of SUDs and MDD can complicate the clinical presentation, making it challenging to differentiate between symptoms of depression, substance withdrawal, or the effects of substance use.
- Integrated Treatment: Dual diagnosis treatment that addresses both MDD and SUDs concurrently is crucial. Integrated interventions consider the interplay of these conditions and provide comprehensive care.
4. Trauma and Comorbidity:
- Trauma History: Individuals with a history of trauma are at an increased risk for both MDD and SUDs. Trauma-focused interventions may be necessary to address underlying factors contributing to comorbidities.
- Trauma-Informed Care: Approaches that recognize the impact of trauma and prioritize safety and empowerment, known as trauma-informed care, are beneficial in treating individuals with comorbid MDD and SUDs.
5. Increased Risk of Relapse:
- Relapse Triggers: The presence of comorbidities increases the risk of relapse in both MDD and SUDs. Identifying and addressing triggers for relapse is essential for sustained recovery.
- Cyclical Nature: The cyclical relationship between depressive episodes and substance use can perpetuate a pattern of chronic relapse if not effectively addressed.
6. Medication Considerations:
- Interactions and Side Effects: When prescribing medications for MDD, consideration of potential interactions with substances is crucial. Some medications may have adverse effects when combined with certain substances.
- Medication Adherence: Individuals with comorbidities may face challenges in adhering to medication regimens. Close monitoring and support are essential for optimizing medication management.
7. Cognitive-Behavioral Interventions:
- Cognitive-Behavioral Therapy (CBT): CBT adapted for individuals with comorbid MDD and SUDs can be effective. It addresses distorted thought patterns, substance use triggers, and provides coping strategies for both conditions.
- Relapse Prevention: CBT-based relapse prevention strategies are particularly important in addressing the risk of relapse in individuals with comorbidities.
8. Social Support and Rehabilitation:
- Rehabilitation Programs: Comprehensive rehabilitation programs that address both MDD and SUDs can provide a structured and supportive environment for individuals with comorbidities.
- Family and Peer Support: Involving family and peer support systems in the treatment process helps create a network of encouragement and accountability.
9. Gradual and Individualized Approach:
- Stepwise Intervention: A stepwise approach to intervention may be necessary, addressing the most acute and life-threatening aspects of both conditions first before delving into deeper therapeutic work.
- Individualized Care Plans: Recognize the individual variability in the interplay of MDD and SUDs. Tailor treatment plans to the unique needs, preferences, and challenges of each individual.
Holistic Treatment Models
The Bio-Psycho-Social Model in Psychiatry
The bio-psycho-social model is a comprehensive framework used in psychiatry to understand and treat mental health disorders, including Major Depressive Disorder (MDD). This model recognizes that biological, psychological, and social factors all play crucial roles in the development, manifestation, and treatment of mental health conditions. Here’s an overview of how the bio-psycho-social model is applied in the treatment of MDD:
1. Biological Factors:
- Neurotransmitter Imbalances: Biological factors in MDD often involve imbalances in neurotransmitters, such as serotonin, norepinephrine, and dopamine. Medications like selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) target these imbalances.
- Genetic Predisposition: There is evidence of a genetic component in MDD. Family history and genetic factors contribute to an individual’s susceptibility to the disorder.
- Neuroendocrine System: Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, which governs the stress response, is associated with MDD. This can lead to elevated cortisol levels, influencing mood and stress sensitivity.
2. Psychological Factors:
- Cognitive Distortions: Psychological factors in MDD include distorted thought patterns, negative self-perception, and cognitive biases. Cognitive-behavioral therapy (CBT) is a widely used psychotherapeutic approach that addresses and corrects these patterns.
- Psychodynamic Influences: Psychodynamic therapies explore unconscious thoughts and past experiences that may contribute to depressive symptoms. Understanding and resolving underlying conflicts can be a focus of treatment.
- Emotion Regulation: Psychological interventions often target emotion regulation strategies, helping individuals develop healthier coping mechanisms and adaptive ways of managing stress.
3. Social Factors:
- Social Support: The absence of a strong social support system or strained interpersonal relationships can contribute to the onset and maintenance of MDD. Building or enhancing social support networks is integral to treatment.
- Life Events and Stressors: Stressful life events, such as loss, trauma, or major life changes, can trigger or exacerbate MDD. Addressing these events and developing coping skills are essential components of treatment.
- Socioeconomic Factors: Social determinants of health, including socioeconomic status, access to education, and employment opportunities, can impact the course of MDD. A comprehensive treatment approach may involve addressing these social factors.
4. Treatment Approaches Using the Bio-Psycho-Social Model:
- Pharmacotherapy: Biological interventions often include antidepressant medications that target neurotransmitter imbalances. The choice of medication is influenced by the individual’s biological profile and response to treatment.
- Psychotherapy: Psychological interventions, such as CBT, psychodynamic therapy, and interpersonal therapy, address cognitive and emotional aspects of MDD. These therapies aim to modify maladaptive thought patterns and improve coping skills.
- Social Interventions: Social interventions involve addressing interpersonal relationships, improving social support, and assisting individuals in navigating social challenges. Family therapy may be beneficial in certain cases.
5. Holistic and Individualized Treatment:
- Integrated Approach: The bio-psycho-social model promotes an integrated treatment approach where biological, psychological, and social factors are considered simultaneously. This may involve collaboration between psychiatrists, psychologists, social workers, and other healthcare professionals.
- Individualized Care Plans: Recognizing the unique interplay of factors in each individual, treatment plans are tailored to address the specific needs, preferences, and challenges of the person with MDD.
6. Prevention and Relapse Prevention:
- Identifying Risk Factors: The bio-psycho-social model is valuable in identifying risk factors for the development of MDD and implementing preventive measures. Recognizing and addressing biological, psychological, and social vulnerabilities can contribute to prevention efforts.
- Comprehensive Relapse Prevention: In ongoing treatment, the model is applied to prevent relapse by addressing biological vulnerabilities through medication management, psychological aspects through continued therapy, and social factors through ongoing support and skill-building.
Incorporating Spirituality in Treatment
Incorporating spirituality into the treatment of Major Depressive Disorder (MDD) recognizes the potential impact of an individual’s spiritual beliefs and practices on mental health and well-being. It’s important to approach this integration with sensitivity, respect for diversity, and collaboration with the individual. Here are ways in which spirituality can be considered in the treatment of MDD:
1. Spiritual Assessment:
- Open and Respectful Inquiry: Begin by engaging in open and respectful conversations about the individual’s spiritual beliefs, values, and practices. A thorough spiritual assessment can provide insight into the role of spirituality in their life.
- Understanding Personal Significance: Explore how spirituality contributes to the person’s sense of purpose, meaning, and connection to something greater than themselves. Understanding the personal significance of spirituality helps tailor treatment approaches.
2. Collaboration with Spiritual Leaders:
- Engaging Religious or Spiritual Leaders: Collaborate with religious or spiritual leaders if the individual is comfortable. Clergy, pastors, imams, or other spiritual figures may offer support, guidance, or counseling within the context of the individual’s faith tradition.
- Integration of Spiritual Practices: Explore ways to integrate spiritual practices, such as prayer, meditation, or rituals, into the individual’s coping strategies. These practices can serve as sources of comfort and resilience.
3. Mindfulness and Meditation:
- Mindfulness-Based Approaches: Mindfulness-based interventions, which have roots in various spiritual traditions, can be adapted to address symptoms of depression. Mindfulness and meditation practices promote present-moment awareness and may contribute to emotional regulation.
- Mindfulness-Based Cognitive Therapy (MBCT): MBCT, which combines mindfulness practices with cognitive-behavioral therapy, has shown effectiveness in preventing the recurrence of depressive episodes.
4. Connection to Community:
- Community Involvement: Encourage involvement in spiritual or religious communities that align with the individual’s beliefs. Connection to a supportive community can provide a sense of belonging and social support, which is valuable in managing MDD.
- Group Activities: Some religious or spiritual communities offer group activities, support groups, or volunteer opportunities. Participation in such activities can enhance social engagement and contribute to a sense of purpose.
5. Values-Based Goal Setting:
- Aligning with Spiritual Values: Collaboratively set treatment goals that align with the individual’s spiritual values and aspirations. Identifying meaningful objectives rooted in spirituality can enhance motivation and a sense of purpose.
- Integrating Values into Therapy: Therapists can integrate spiritual values into therapeutic techniques, such as cognitive-behavioral therapy (CBT) or solution-focused therapy, to make the treatment more relevant and personally meaningful.
6. Addressing Existential Concerns:
- Exploring Existential Questions: Individuals with MDD may grapple with existential questions related to purpose, suffering, and the nature of life. Therapists can provide a space to explore and process these existential concerns within the context of the individual’s spirituality.
- Existential and Logotherapy Approaches: Drawing from existential or logotherapy principles, therapists can help individuals find meaning and purpose in their experiences, aligning with their spiritual perspectives.
7. Respect for Diversity:
- Cultural Sensitivity: Be culturally sensitive and respectful of diverse spiritual and religious beliefs. Recognize that individuals may have different faith traditions or spiritual practices, and tailor interventions accordingly.
- Inclusive Language: Use inclusive language that respects and honors the individual’s spiritual beliefs without imposing specific religious or spiritual perspectives.
8. Ethical Considerations:
- Informed Consent: Obtain informed consent before incorporating spirituality into treatment. Ensure that the individual is comfortable with the integration of spiritual elements and that it aligns with their values.
- Respecting Boundaries: Be mindful of ethical considerations, respecting the individual’s boundaries and avoiding coercion or imposition of specific spiritual beliefs.
The Importance of Family and Social Support

Family and social support play a crucial role in the treatment of Major Depressive Disorder (MDD). Building a strong support system can significantly enhance the effectiveness of therapeutic interventions and contribute to the overall well-being of individuals with MDD. Here are key aspects highlighting the importance of family and social support in the treatment of MDD:
1. Emotional Support:
- Understanding and Empathy: Family and social support systems can provide understanding and empathy, helping individuals with MDD feel heard and validated. Emotional support fosters a sense of connection and reduces feelings of isolation.
- Validation of Feelings: Knowing that family and friends acknowledge the challenges of MDD and validate the individual’s feelings can contribute to a supportive and nurturing environment.
2. Treatment Engagement:
- Encouraging Treatment Seeking: Supportive family and friends can play a vital role in encouraging individuals to seek professional help for MDD. Their encouragement and assistance in accessing mental health services can be a significant motivator.
- Collaborative Decision-Making: Involving family members in treatment decisions, with the individual’s consent, enhances collaboration and ensures a more comprehensive approach to recovery.
3. Monitoring Medication and Treatment Adherence:
- Assistance with Medication Management: Family members can assist in monitoring medication adherence, especially if the individual is prescribed antidepressant medication. Support in maintaining a consistent medication routine is crucial for treatment effectiveness.
- Encouraging Therapy Attendance: Family and social support can help reinforce the importance of attending therapy sessions. Encouragement to participate in psychotherapy contributes to the therapeutic process.
4. Practical Support:
- Assistance with Daily Tasks: Individuals with MDD may find daily tasks challenging. Family and friends can provide practical support, such as assistance with household chores, meal preparation, or childcare, alleviating some of the stressors.
- Creating a Supportive Environment: A supportive home environment, where individuals feel safe and cared for, can positively impact their mental well-being.
5. Recognition of Warning Signs:
- Early Detection of Symptoms: Close friends and family are often the first to notice changes in behavior or mood. Their awareness of warning signs allows for early detection of symptoms and timely intervention.
- Communication with Healthcare Providers: Encouraging open communication between the individual, family, and healthcare providers facilitates a collaborative approach to treatment and enables timely adjustments to the treatment plan.
6. Prevention of Isolation:
- Combatting Social Isolation: Depression often leads to social withdrawal and isolation. Family and social support networks provide opportunities for individuals to engage in social activities, reducing feelings of loneliness.
- Inclusion in Social Gatherings: Including individuals with MDD in social gatherings, even on a small scale, promotes a sense of belonging and normalcy.
7. Education and Understanding:
- Promoting Mental Health Literacy: Families and friends benefit from education about MDD, including its symptoms, causes, and treatment options. Increased understanding reduces stigma and fosters a supportive atmosphere.
- Communication Skills Training: Learning effective communication skills helps family members and friends engage in supportive conversations without judgment, fostering an open and compassionate environment.
8. Relapse Prevention:
- Ongoing Support Post-Treatment: Family and social support are essential in the post-treatment phase to help prevent relapse. Continued emotional support and encouragement contribute to the individual’s long-term well-being.
- Recognition of Triggers: With awareness of potential triggers, family and friends can play a role in helping individuals navigate stressors and challenges that may contribute to a recurrence of depressive symptoms.
9. Community Resources:
- Connecting with Support Groups: In addition to family support, individuals with MDD can benefit from participation in support groups or community resources. These provide additional avenues for understanding, shared experiences, and encouragement.
10. Resilience Building:
- Promoting Resilience: Supportive relationships contribute to the development of resilience in individuals with MDD. Encouragement, reinforcement of strengths, and recognition of progress contribute to a more positive outlook.
Challenges in Treatment Adherence
Stigma Associated with Mental Health Treatment
Stigma associated with mental health treatment, particularly for Major Depressive Disorder (MDD), is a pervasive and damaging societal issue that can act as a barrier to seeking help, hinder recovery, and perpetuate misconceptions about mental health. Understanding and addressing this stigma are essential steps in promoting a more supportive and inclusive environment for individuals affected by MDD. Here are key aspects of the stigma associated with mental health treatment, specifically MDD:
1. Social Stigma:
- Negative Stereotypes: Stigma surrounding MDD often involves negative stereotypes and misconceptions about individuals with depression. Common stereotypes include seeing them as lazy, weak, or lacking in willpower.
- Fear of Judgment: Individuals with MDD may fear judgment from others, leading to reluctance in disclosing their condition or seeking help. This fear can contribute to social isolation and hinder the development of a supportive network.
2. Self-Stigma:
- Internalized Shame: Individuals with MDD may internalize societal stigma, experiencing feelings of shame or inadequacy. This self-stigma can undermine self-esteem and confidence, further complicating the journey to recovery.
- Impact on Self-Help-Seeking: Internalized stigma may lead to delays in seeking professional help. The fear of being labeled or judged can prevent individuals from acknowledging their need for support.
3. Barriers to Treatment:
- Treatment Avoidance: Stigma contributes to the avoidance of mental health treatment, including therapy and medication. Individuals may hesitate to pursue help due to concerns about how they will be perceived by others.
- Impact on Treatment Adherence: Even when individuals initiate treatment, stigma can affect treatment adherence. The fear of being associated with a mental health diagnosis may lead to discontinuation of treatment prematurely.
4. Workplace Stigma:
- Professional Consequences: Fear of professional consequences, such as discrimination or stigmatization at work, may prevent individuals from disclosing their mental health condition to employers or seeking necessary accommodations.
- Productivity and Stigma: The belief that individuals with MDD may be less productive or reliable at work due to stigma can create a hostile work environment, perpetuating discrimination.
5. Cultural Stigma:
- Cultural Beliefs: Cultural factors can influence stigma, with some cultures attaching shame or disgrace to mental health conditions. Cultural misconceptions about the causes and treatment of MDD may impact help-seeking behavior.
- Lack of Cultural Competence: Limited cultural competence within healthcare systems can exacerbate stigma, making it challenging for individuals from diverse backgrounds to access culturally sensitive mental health care.
6. Media Representation:
- Stigmatizing Portrayals: Media portrayals of mental health conditions, including MDD, can perpetuate stigmatizing stereotypes and contribute to public misconceptions. Accurate and compassionate representations are crucial for challenging these stereotypes.
- Impact on Public Perception: Misleading media representations may shape public attitudes, influencing how MDD is perceived and reinforcing stigmatizing beliefs.
7. Advocacy and Education:
- Challenging Stigma Through Education: Public awareness campaigns and educational initiatives can challenge stereotypes, correct misconceptions, and promote understanding about MDD and mental health in general.
- Personal Stories and Advocacy: Sharing personal stories of individuals who have experienced MDD and recovery can humanize the condition, reduce stigma, and encourage empathy.
8. Policy and Legal Frameworks:
- Anti-Discrimination Measures: Implementing and enforcing anti-discrimination measures in workplaces and healthcare settings helps protect individuals with MDD from stigma-related discrimination.
- Legislation and Mental Health Parity: Advocating for legislation that supports mental health parity, ensuring equitable access to mental health treatment, can contribute to reducing stigma and improving treatment accessibility.
9. Mental Health First Aid:
- Training Programs: Mental Health First Aid training programs teach individuals how to provide initial support to someone experiencing a mental health crisis, fostering empathy and reducing stigma.
- Normalizing Conversations: Open and normalized conversations about mental health in various settings, such as schools and workplaces, can contribute to reducing stigma and creating a culture of acceptance.
Addressing Medication Noncompliance
Addressing medication noncompliance in the treatment of Major Depressive Disorder (MDD) is crucial for optimizing therapeutic outcomes and supporting individuals on their journey to recovery. Noncompliance with antidepressant medication can be influenced by various factors, and a tailored and collaborative approach is essential. Here are key strategies to address medication noncompliance in the treatment of MDD:
1. Therapeutic Alliance:
- Build a Trusting Relationship: Establishing a trusting and collaborative relationship between the individual and the healthcare provider is fundamental. Open communication and a supportive therapeutic alliance create a foundation for addressing noncompliance.
- Understanding Concerns: Explore the individual’s concerns and beliefs about medication. Understanding their perspective helps tailor interventions to address specific barriers to compliance.
2. Education and Psychoeducation:
- Provide Comprehensive Information: Educate individuals about the nature of MDD, the role of medication in treatment, and the expected benefits. Clear and comprehensive information helps demystify the treatment process and enhances informed decision-making.
- Addressing Misconceptions: Correct any misconceptions or myths about antidepressant medications. Address concerns related to side effects, dependency, or stigma associated with taking medication for mental health.
3. Shared Decision-Making:
- Involve Individuals in Treatment Decisions: Engage individuals in shared decision-making regarding their treatment plan. When individuals actively participate in decisions about their care, they are more likely to feel a sense of ownership and commitment to the treatment.
- Tailor Treatment Plans: Collaboratively tailor treatment plans to meet individual preferences and lifestyle factors. Taking into account personal preferences can contribute to better adherence.
4. Simplified Medication Regimen:
- Simplify Dosage Schedule: Work with healthcare providers to simplify the medication regimen whenever possible. Reducing the frequency of dosages or adjusting the timing of medication administration can enhance adherence.
- Consider Extended-Release Formulations: Extended-release formulations, if available, may be considered to minimize the frequency of daily dosing, making it more manageable for individuals.
5. Side Effect Management:
- Proactive Side Effect Management: Anticipate and address potential side effects proactively. Discuss common side effects, their expected duration, and strategies for managing them. This proactive approach can alleviate concerns and improve tolerance.
- Medication Adjustment: If side effects are a significant barrier, collaborate with healthcare providers to explore potential adjustments to the medication dosage or consider alternative medications with a more favorable side effect profile.
6. Regular Monitoring and Follow-ups:
- Scheduled Follow-ups: Schedule regular follow-up appointments to monitor treatment progress and assess for any emerging issues. Regular check-ins provide opportunities to discuss experiences with the medication, address concerns, and make necessary adjustments.
- Monitoring Response to Treatment: Regularly monitor and discuss the individual’s response to treatment. Highlight positive changes and improvements related to medication compliance to reinforce the benefits.
7. Addressing Mental Health Literacy:
- Enhance Mental Health Literacy: Improve mental health literacy by providing educational resources and materials. Increasing awareness and understanding of the importance of medication in treating MDD can positively impact compliance.
- Incorporate Psychoeducation: Integrate psychoeducation into therapy sessions, focusing on the neurobiological aspects of depression and how medication contributes to symptom relief. This knowledge empowers individuals to make informed choices about their treatment.
8. Involvement of Support System:
- Engage Family and Supportive Individuals: If appropriate and with the individual’s consent, involve family members or supportive individuals in discussions about medication adherence. Their understanding and encouragement can play a supportive role.
- Educate Support System: Provide education to the support system about the importance of medication adherence in MDD treatment. Address any misconceptions or concerns they may have.
9. Technology and Reminders:
- Use of Technology: Leverage technology, such as medication reminder apps, to help individuals stay on track with their medication schedule. These tools can provide reminders and support adherence.
- Pill Organizers: Recommend the use of pill organizers to help individuals organize their medication and track whether doses have been taken. This visual aid can be a simple yet effective strategy.
10. Addressing Barriers Outside of Medication:
- Identify and Address Barriers: Explore potential barriers to adherence that extend beyond the medication itself, such as financial constraints, transportation issues, or other life stressors. Collaborate on solutions to address these challenges.
- Integrate Non-Pharmacological Approaches: Emphasize the importance of a holistic treatment approach that may include psychotherapy, lifestyle modifications, and support from a multidisciplinary team. Combining medication with non-pharmacological interventions can enhance overall treatment effectiveness.
11. Emergency Response Plan:
- Emergency Protocols: Discuss emergency response plans with individuals, including steps to take if they miss doses or experience a crisis. Having a clear plan in place helps individuals feel more in control and supported.
- Crisis Helplines: Provide information about crisis helplines and resources for immediate support in case of emergent situations. Ensuring individuals are aware of available resources can be a crucial safety measure.
Integrating Technology for Better Adherence
Integrating technology for better adherence in the treatment of Major Depressive Disorder (MDD) can be both an opportunity and a challenge. While technology offers innovative solutions to enhance medication adherence and support mental health, there are also associated challenges that need careful consideration. Here are key aspects to navigate when integrating technology for better adherence in the treatment of MDD:
1. Opportunities:
- Medication Reminder Apps: Develop or recommend medication reminder apps that send notifications to individuals at scheduled times for medication administration. These apps can improve adherence by providing a convenient and automated reminder system.
- Telehealth and Virtual Check-Ins: Utilize telehealth platforms for virtual check-ins and consultations. Virtual appointments can enhance accessibility, especially for individuals facing transportation or scheduling challenges, promoting ongoing engagement with healthcare providers.
- Digital Health Platforms: Implement digital health platforms that allow individuals to track their medication adherence, mood, and other relevant data. These platforms can provide valuable insights for healthcare providers and facilitate collaborative decision-making.
2. Challenges:
- Technological Literacy: Some individuals, particularly older adults or those with limited access to technology, may face challenges in using digital tools. Addressing technological literacy barriers requires providing guidance and support for effective use.
- Privacy and Security Concerns: Privacy and security concerns regarding health data may impact individuals’ willingness to use technology for mental health treatment. Ensuring robust data protection measures and transparent communication about privacy can mitigate these concerns.
- Access to Technology: Disparities in access to smartphones, tablets, or the internet may create inequities in the use of technology for mental health support. Consideration must be given to individuals who may not have reliable access to digital devices.
3. Solutions:
- Education and Training: Provide education and training on the use of technology for mental health management. This includes offering tutorials, user-friendly guides, and ongoing support to enhance individuals’ confidence and proficiency.
- Tailored Technology Solutions: Consider individual preferences and needs when recommending or implementing technology solutions. Offering a range of options, such as apps with customizable features, accommodates diverse user preferences.
- Addressing Privacy Concerns: Clearly communicate the security measures in place to protect individuals’ privacy. Emphasize compliance with health information protection regulations and ethical standards, fostering trust in the use of technology.
4. Remote Monitoring:
- Remote Medication Monitoring: Explore technologies that enable remote monitoring of medication adherence. Smart pill dispensers or connected devices can provide real-time data to healthcare providers, allowing for timely interventions if adherence issues arise.
- Wearable Devices: Consider the use of wearable devices that track physical activity, sleep patterns, and stress levels. Integrating this data into treatment plans can provide a more comprehensive understanding of an individual’s well-being.
5. Teletherapy and Support Groups:
- Virtual Support Groups: Facilitate virtual support groups for individuals with MDD. Technology can connect individuals facing similar challenges, providing a sense of community and shared experiences, which can positively impact adherence.
- Teletherapy Platforms: Integrate teletherapy platforms for remote counseling sessions. This approach enhances accessibility to mental health professionals and allows for consistent therapeutic support.
6. User-Centered Design:
- User-Centered App Design: Prioritize user-centered design principles when developing medication adherence apps. Ensure that the interface is intuitive, visually appealing, and accommodates various user preferences to enhance engagement.
- Feedback and Iterative Improvement: Solicit feedback from users about their experience with technology-based interventions. Continuously iterate and improve digital tools based on user input to enhance usability and effectiveness.
7. Collaboration with Healthcare Providers:
- Healthcare Provider Training: Train healthcare providers on incorporating technology into their practice. This includes guidance on using telehealth platforms effectively and interpreting data from digital health tools to inform treatment decisions.
- Integration into Electronic Health Records (EHRs): Integrate data from technology-based adherence tools into electronic health records (EHRs). This integration ensures seamless communication between healthcare providers and allows for a more comprehensive view of an individual’s health.
8. Cultural Sensitivity:
- Cultural Adaptation: Ensure that technology-based interventions are culturally sensitive and consider diverse cultural backgrounds. This includes language preferences, cultural norms, and beliefs about mental health and technology.
- Accessibility Features: Incorporate accessibility features into digital tools to accommodate individuals with diverse needs, including those with visual or hearing impairments.
Conclusion
In conclusion, Major Depressive Disorder (MDD) is a complex and pervasive mental health condition that significantly impacts individuals’ well-being, functioning, and overall quality of life. As we explore the various aspects of MDD, it is evident that a comprehensive understanding and approach are crucial for effective diagnosis, treatment, and support. Here are key takeaways:
1. Recognition and Diagnosis:
- Diagnostic Criteria: Accurate diagnosis of MDD involves careful consideration of specific criteria outlined in standardized diagnostic manuals, such as the DSM-5.
- Clinical Assessment: Thorough clinical assessment, including a detailed examination of symptoms, duration, and functional impairment, is essential for an accurate diagnosis.
2. Impact on Individuals and Society:
- Personal and Social Consequences: MDD profoundly affects individuals, impacting their emotional well-being, relationships, and daily functioning.
- Societal Burden: The societal burden of MDD is substantial, encompassing economic costs, decreased productivity, and challenges in interpersonal relationships.
3. Treatment Modalities:
- Biological, Psychological, and Social Factors: The bio-psycho-social model provides a holistic framework for understanding and treating MDD, recognizing the interplay of biological, psychological, and social factors.
- Pharmacotherapy: Antidepressant medications play a key role in addressing neurobiological aspects of MDD by targeting neurotransmitter imbalances.
- Psychotherapy: Various psychotherapeutic approaches, such as Cognitive-Behavioral Therapy (CBT) and psychodynamic therapy, address cognitive and emotional aspects of MDD.
- Innovative Interventions: Emerging interventions, including transcranial magnetic stimulation (TMS) and ketamine treatment, show promise in cases of treatment-resistant depression.
4. Challenges and Considerations:
- Stigma: Stigma associated with MDD remains a significant barrier to seeking help and receiving adequate support. Education, awareness, and destigmatization efforts are essential.
- Medication Noncompliance: Addressing challenges related to medication noncompliance involves fostering a trusting therapeutic alliance, providing education, and utilizing technology for support.
5. Holistic Approaches:
- Incorporating Technology: Integrating technology into MDD treatment offers opportunities for improved adherence, telehealth, and remote monitoring. However, addressing issues of access, privacy, and user-centered design is crucial.
- Spirituality and Social Support: Recognizing the importance of spirituality and involving family and social support networks are integral for a holistic approach to MDD treatment.
6. Future Directions:
- Research and Innovation: Ongoing research continues to deepen our understanding of MDD and inform innovative treatment approaches. Advances in neuroscience, genetics, and personalized medicine hold promise for more targeted interventions.
- Mental Health Advocacy: Advocacy efforts are crucial for challenging stigma, promoting mental health literacy, and ensuring equitable access to effective treatments.