Tania Douglas is a 36-year-old attorney living in Miami. Dolores is in the second trimester of pregnancy with her first child, and though her pregnancy had been progressing normally
EXPERT ANSWER AND EXPLANATION
Iron Deficiency Anemia (IDA)
Definition and Etiology
Camaschella (2017) posits that this is a disorder of the hematological system that results from inadequate iron supply to the bone marrow, with resultant impaired production of red blood cells along with deficient hemoglobinization. The resultant cells are therefore described as being microcytic and hypochromic, on the basis of the red blood cell indices as will be elucidated later. Notably, the extent of hypochromia and microcytosis corresponds to the chronicity and severity of the disease.
Four major mechanisms, according to Hoffbrand & Moss (2015), are postulated to bear implications in the etiology, pathogenesis and subsequent course of iron deficiency anemia. This includes inadequate dietary intake of iron, impaired absorption of iron, increased losses and enhanced demand. Illnesses and socioeconomic factors contribute to inadequate feeding and thus deficiency while 8malabsorption is usually secondary to small bowel disorders and/or extensive bowel surgeries. Hemorrhage contributes to significant iron losses, while pregnancy is one of the states of increased demand (Hoffbrand & Moss, 2015).
Diagnostics
While the diagnosis of anemia is commonly made clinically, assessment of the specific type of anemia as well as severity needs laboratory diagnosis (Wu, Lesperance & Bernstein, 2016). As part of the initial diagnosis, performing complete blood count (CBC), bone marrow aspiration and iron studies.
CBC provides information on the red cell indices and the state of other blood cell lines, which is important in knowing whether it is a pancytopenic process. Iron studies involves doing serum iron levels, serum ferritin and transferrin. The former is usually low while the remaining two are usually elevated (Wu, Lesperance & Bernstein, 2016). Bone marrow aspiration aids in gauging the marrow response to the anemia as well as assessing iron stores. Further tests to be done regarding etiology include stool culture and endoscopic procedures.
Significance of Red Blood Cell Indices
Red blood cell indices, as a component of complete blood count, provides a fast, easy to do laboratory technique of assessing the severity of anemia as well as (Wu, Lesperance & Bernstein, 2016). Iron deficiency anemia is associated with characteristic changes in the red cell morphology, size, hemoglobin content and number, and this is manifested in the indices as microcytosis, hypochromia and reduced absolute numbers of red cells.
Treatment and Prevention
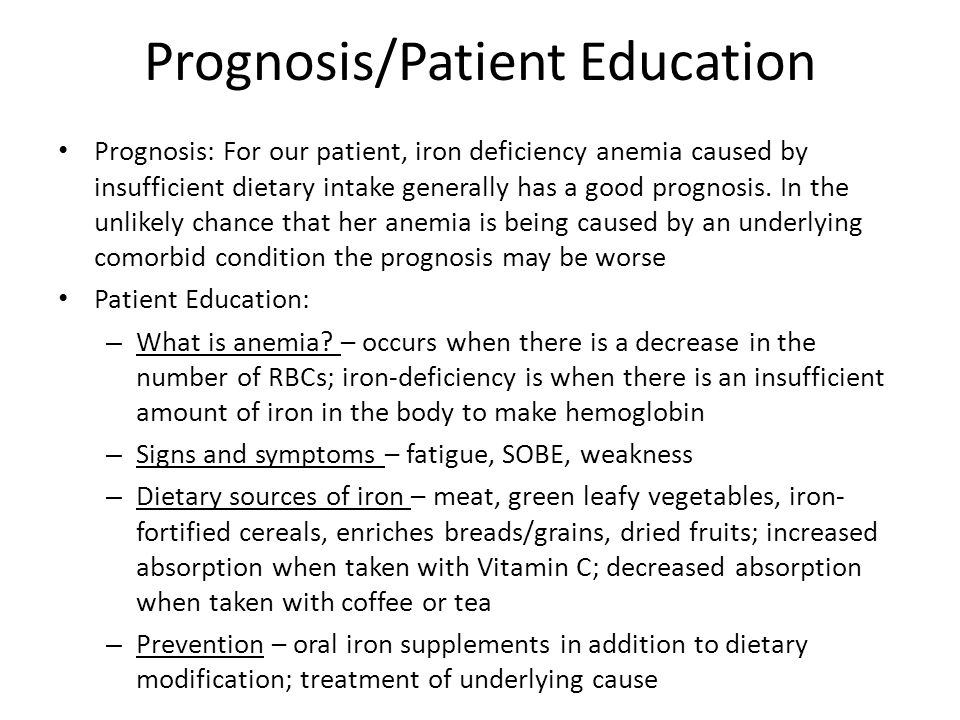
According to Cantor et al. (2015) prevention of the disorder involves observance of hygienic dietary practices such as washing foods well enough as well periodic deworming of the at risk groups, feeding practices which should also revolve around iron rich foods such as spinach and meat and for pregnant women, IFAS should be provided and taken as prescribed.
Therapy varies depending on severity, where oral iron supplementation is provided for mild to moderate cases in form of ferrous sulphate or gluconate, whereas parenteral iron is given for acute severe cases. In even more demanding scenarios, transfusion is recommended (Cantor et al., 2015).
Patient Education
IDA is the most prevalent anemia and educating the masses is an integral part of ensuring control and proper management of the disorder (DeLoughery, 2017). Measures patients should be taught include:
- Encouraging deworming for under 5 year old children as well as at risk adults.
- Healthy feeding practices involving eating iron rich foods such as fruits and vegetables.
- Prompt treatment and prevention of malaria in pregnancy in endemic areas.
- Advising taking of IFAS by pregnant women as prescribed by the practitioner.
References
Camaschella, C. (2017). New insights into iron deficiency and iron deficiency anemia. Blood reviews, 31(4), 225-233.
Cantor, A. G., Bougatsos, C., Dana, T., Blazina, I., & McDonagh, M. (2015). Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the US Preventive Services Task Force. Annals of internal medicine, 162(8), 566-576.
DeLoughery, T. G. (2017). Iron deficiency anemia. Medical Clinics, 101(2), 319-332.
Hoffbrand, A. V., & Moss, P. A. (2015). Hoffbrand’s essential haematology (Vol. 38). John Wiley & Sons.
Wu, A. C., Lesperance, L., & Bernstein, H. (2016). Screening for iron deficiency. Policy Statement, 23, 171-177.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Use Coupon Code: NEW30 to Get 30% OFF Your First Order
What is the main cause of IDA?
The main cause of Iron Deficiency Anemia (IDA) is a deficiency of iron in the body. Iron is a vital mineral that plays a crucial role in the production of hemoglobin, a protein in red blood cells that carries oxygen from the lungs to the rest of the body. When there is insufficient iron available, the body cannot produce an adequate amount of hemoglobin, which can lead to anemia.
There are several common factors and conditions that can contribute to iron deficiency anemia:
- Inadequate Dietary Intake: A diet that lacks sufficient iron-rich foods can lead to iron deficiency. This is more common in individuals who do not consume enough iron from sources such as red meat, poultry, fish, beans, lentils, fortified cereals, and leafy green vegetables.
- Blood Loss: The most common cause of iron deficiency anemia is blood loss, which can occur from various sources:
- Gastrointestinal Bleeding: Conditions like ulcers, gastritis, or colorectal cancer can lead to chronic bleeding in the digestive tract, resulting in iron loss.
- Menstruation: Women with heavy menstrual bleeding are at an increased risk of developing iron deficiency anemia.
- Internal Bleeding: Injuries, surgeries, or certain medical conditions can cause internal bleeding, leading to iron loss.
- Poor Iron Absorption: Some medical conditions can interfere with the body’s ability to absorb iron efficiently. These conditions include celiac disease, inflammatory bowel disease (IBD), and certain medications that affect the gastrointestinal tract.
- Pregnancy and Breastfeeding: Pregnant and breastfeeding women require higher amounts of iron to support the growing fetus or infant. If dietary intake or supplementation is inadequate, it can lead to iron deficiency anemia.
- Chronic Illnesses: Certain chronic medical conditions, such as chronic kidney disease, cancer, and autoimmune disorders, can disrupt iron metabolism and lead to iron deficiency anemia.
- Dietary Restrictions: Vegetarians and vegans may be at a higher risk of iron deficiency anemia because plant-based sources of iron (non-heme iron) are not as readily absorbed by the body as heme iron found in animal products.
- Blood Donation: Frequent blood donation or blood loss due to blood disorders can deplete iron stores over time and lead to anemia.
It’s important to recognize the underlying cause of iron deficiency anemia, as treatment may vary depending on the specific factor contributing to the deficiency. Diagnosis typically involves blood tests to measure hemoglobin levels, serum iron, ferritin (a protein that stores iron), and other markers of iron status. Treatment may involve iron supplements, dietary changes, and addressing the underlying cause of the deficiency, such as treating gastrointestinal bleeding or managing chronic illnesses. Consulting a healthcare professional is crucial for an accurate diagnosis and appropriate management of iron deficiency anemia.
What is the meaning of IDA in anemia?
In the context of anemia, “IDA” stands for “Iron Deficiency Anemia.” Iron Deficiency Anemia is a common type of anemia characterized by a deficiency of iron in the body. This condition occurs when the body lacks an adequate supply of iron, which is essential for the production of hemoglobin—a protein in red blood cells responsible for carrying oxygen from the lungs to the rest of the body.
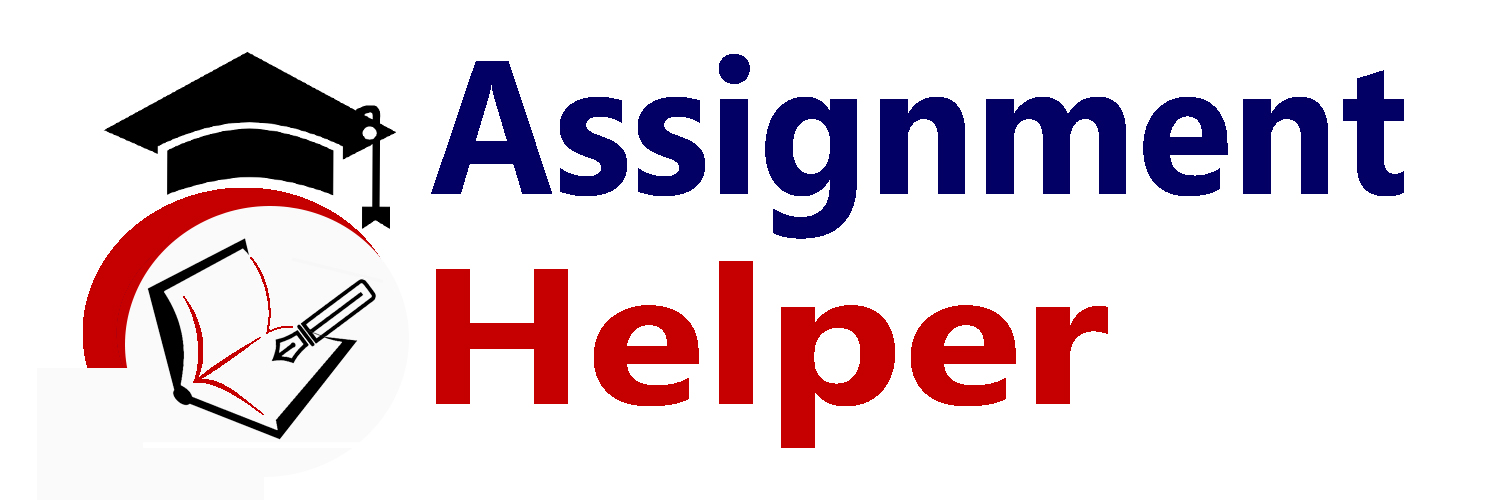
When there is insufficient iron available, the body cannot produce an adequate amount of hemoglobin, resulting in a decreased ability to transport oxygen. This can lead to various symptoms of anemia, including fatigue, weakness, pale skin, shortness of breath, and a decreased ability to perform physical activities.
IDA is one of the most prevalent forms of anemia globally and can be caused by factors such as inadequate dietary iron intake, blood loss due to injury or medical conditions, poor iron absorption, and other underlying health issues. It is important to diagnose and treat Iron Deficiency Anemia, as it can have a significant impact on an individual’s overall health and quality of life. Treatment typically involves iron supplementation, dietary changes, and addressing the underlying cause of the iron deficiency when necessary.
5 weird signs of iron deficiency
Iron deficiency can manifest in various unusual and sometimes unexpected ways beyond the typical symptoms of fatigue and pale skin. Here are five weird signs of iron deficiency:
- Pica:
- One unusual symptom of iron deficiency is a condition called pica. People with pica have a strong craving for non-food items, such as ice, dirt, clay, chalk, or paper. This craving for non-nutritive substances can be a sign of an underlying iron deficiency.
- Restless Leg Syndrome (RLS):
- Restless Leg Syndrome is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations like tingling or crawling. Iron deficiency has been linked to the development or worsening of RLS symptoms. Treating the underlying iron deficiency can sometimes alleviate RLS symptoms.
- Koilonychia (Spoon-Shaped Nails):
- Koilonychia is a condition where the nails become concave and appear spoon-shaped. This unusual nail deformity can be associated with iron deficiency anemia.
- Painful Swallowing:
- In some cases, iron deficiency can lead to a condition known as Plummer-Vinson syndrome or Paterson-Kelly syndrome. One of the peculiar symptoms of this syndrome is the development of painful swallowing or a sensation of food getting stuck in the throat.
- Hair Loss:
- While hair loss can be a more commonly recognized symptom of iron deficiency, it can sometimes manifest in unusual patterns. In some cases, people with iron deficiency may experience hair loss not just on the scalp but also in other body areas, including eyebrows and eyelashes.
What are the 3 stages of iron deficiency?
Iron deficiency typically progresses through several stages, each with its own set of symptoms and severity. The three main stages of iron deficiency are as follows:
- Stage 1: Iron Depletion (Iron Deficient Stores):
- In the initial stage, the body’s iron stores become depleted. However, the individual may not yet experience significant symptoms.
- Laboratory tests may show a decrease in serum ferritin levels, which is a protein that stores iron. Ferritin levels are often used as an indicator of iron stores in the body.
- At this stage, hemoglobin levels, which are used to diagnose anemia, may still be within the normal range. Therefore, individuals may not yet meet the criteria for anemia.
- Stage 2: Iron-Deficient Erythropoiesis (Functional Iron Deficiency):
- In this stage, iron deficiency progresses, and the body begins to struggle to produce enough healthy red blood cells (erythropoiesis).
- As iron reserves continue to deplete, symptoms may become more noticeable. These can include fatigue, weakness, pale skin, and a decreased ability to tolerate physical activity.
- Laboratory tests may reveal lower levels of serum iron and transferrin saturation, along with reduced hemoglobin levels. These findings indicate a functional iron deficiency, meaning the body is having difficulty supplying enough iron to support the production of red blood cells.
- Stage 3: Iron Deficiency Anemia:
- This is the most advanced stage of iron deficiency, characterized by a significant decrease in hemoglobin levels. Hemoglobin is the protein in red blood cells that carries oxygen throughout the body.
- As hemoglobin levels drop, the classic symptoms of anemia become more pronounced. These can include extreme fatigue, weakness, pale or yellowish skin, shortness of breath, dizziness, and cold extremities.
- Laboratory tests will confirm the presence of anemia, typically defined as a hemoglobin level below a certain threshold for a person’s age and sex.
- Other blood markers, such as mean corpuscular volume (MCV) and mean corpuscular hemoglobin concentration (MCHC), may also indicate the presence of anemia.
Pathophysiology of iron deficiency anemia
Iron deficiency anemia (IDA) is a common type of anemia characterized by a deficiency of iron in the body. Understanding the pathophysiology of IDA involves recognizing how iron is normally utilized in the body, how its deficiency affects various processes, and the resulting clinical manifestations. Here’s an overview of the pathophysiology of IDA:
- Iron Absorption and Intake:
- Iron is primarily obtained through dietary intake. It is absorbed in the small intestine, mainly in the duodenum and upper jejunum.
- In a healthy individual, dietary iron is absorbed as both heme iron (found in animal sources) and non-heme iron (found in plant-based sources).
- Iron Transport and Storage:
- Once absorbed, iron is transported in the blood bound to transferrin, a carrier protein.
- Iron is stored in the body primarily in the form of ferritin, a protein that acts as an iron reservoir, particularly in the liver, spleen, and bone marrow.
- Iron Utilization in Hemoglobin:
- Iron plays a central role in the production of hemoglobin, the protein in red blood cells responsible for carrying oxygen.
- Iron is incorporated into the heme portion of hemoglobin, allowing red blood cells to efficiently transport oxygen from the lungs to tissues throughout the body.
- Pathophysiology of Iron Deficiency Anemia:
- Iron deficiency anemia occurs when there is an insufficient supply of iron to meet the body’s demands for hemoglobin synthesis.
- Depletion of iron stores (reduced ferritin levels) is typically the initial stage of IDA.
- As iron stores become inadequate, the body starts to prioritize the allocation of the limited iron to essential functions, such as maintaining normal cellular function. However, this means that there is not enough iron available for the production of new red blood cells.
- Without adequate iron, the bone marrow struggles to produce enough hemoglobin, leading to the development of smaller and paler red blood cells (microcytic and hypochromic).
- Reduced hemoglobin levels result in diminished oxygen-carrying capacity of red blood cells, leading to tissue hypoxia (insufficient oxygen supply to body tissues).
- Clinical Manifestations:
- The clinical manifestations of iron deficiency anemia include fatigue, weakness, pallor (pale skin), shortness of breath, dizziness, and cold extremities.
- In severe cases, individuals may experience brittle nails, spoon-shaped nails (koilonychia), a sore or inflamed tongue (glossitis), and unusual cravings for non-food items (pica).
- Causes of Iron Deficiency:
- Iron deficiency can result from various factors, including inadequate dietary iron intake, chronic blood loss (due to conditions such as gastrointestinal bleeding or heavy menstruation), poor iron absorption (associated with certain medical conditions like celiac disease or inflammatory bowel disease), and increased iron demands (such as during pregnancy or rapid growth periods in children).
Treatment of iron deficiency anemia typically involves iron supplementation to replenish iron stores, dietary modifications to increase iron intake, and addressing any underlying causes or conditions contributing to the deficiency. Early diagnosis and treatment are essential to prevent complications and improve overall health and well-being.
Iron deficiency anemia treatments
The treatment of iron deficiency anemia (IDA) focuses on replenishing iron stores in the body, addressing the underlying cause of the deficiency, and managing the associated symptoms. Here are the key components of treatment for IDA:
- Iron Supplementation:
- The most common and effective treatment for IDA is oral iron supplementation. Iron supplements are available over-the-counter and by prescription.
- Ferrous sulfate, ferrous gluconate, and ferrous fumarate are commonly prescribed forms of iron supplements.
- It’s essential to take iron supplements as directed by a healthcare professional, typically on an empty stomach or with vitamin C to enhance absorption. Avoid taking them with dairy products, tea, or coffee, as these can hinder iron absorption.
- Iron supplements may cause side effects such as constipation, nausea, and stomach upset. If side effects are intolerable, a healthcare provider may recommend switching to a different iron preparation.
- Dietary Changes:
- In addition to iron supplementation, dietary changes can help increase iron intake. It’s advisable to consume iron-rich foods, including:
- Red meat, poultry, and fish (heme iron sources)
- Legumes, lentils, tofu, and fortified cereals (non-heme iron sources)
- Dark leafy greens, such as spinach and kale
- Nuts and seeds
- Dried fruits, such as raisins and apricots
- Iron-fortified foods, like breakfast cereals
- Combining iron-rich foods with vitamin C-rich foods (e.g., citrus fruits, bell peppers) can enhance iron absorption.
- In addition to iron supplementation, dietary changes can help increase iron intake. It’s advisable to consume iron-rich foods, including:
- Addressing Underlying Causes:
- Treatment should also focus on identifying and addressing the underlying cause of iron deficiency, such as gastrointestinal bleeding, heavy menstrual bleeding, or an underlying medical condition.
- Treating the root cause is essential to prevent recurrent iron deficiency.
- Blood Transfusion:
- In severe cases of IDA where an individual’s hemoglobin levels are dangerously low, or if they experience symptoms of severe anemia like chest pain or shortness of breath, a blood transfusion may be necessary to rapidly increase hemoglobin levels.
- Managing Symptoms:
- Healthcare providers may recommend medications to manage specific symptoms associated with IDA, such as pain relievers for headache or menstrual pain.
- Fatigue and weakness can take time to improve, but they often do so gradually as iron stores are replenished.
- Regular Follow-Up:
- Individuals with IDA typically require regular follow-up with their healthcare provider to monitor their response to treatment. This may involve periodic blood tests to check hemoglobin levels and iron status.
- Adjustments to treatment may be made based on the individual’s progress.
- Prevention:
- Preventing iron deficiency anemia involves maintaining a balanced diet that includes iron-rich foods, managing conditions that can lead to chronic blood loss, and addressing iron deficiency promptly when it occurs.
It’s crucial to consult a healthcare provider for a proper diagnosis and tailored treatment plan for iron deficiency anemia. Self-diagnosis and treatment without medical guidance can be ineffective and may lead to other health complications. Additionally, if IDA is recurrent or persistent, further evaluation may be needed to rule out underlying health conditions.
Iron deficiency anemia diagnosis
Diagnosing iron deficiency anemia (IDA) involves a series of medical assessments and tests conducted by a healthcare provider. The process typically includes the following steps:
- Medical History and Physical Examination:
- The healthcare provider will begin by taking a detailed medical history, including questions about symptoms, diet, menstrual cycle (for females), and any underlying medical conditions.
- A physical examination may be performed to assess for signs of anemia, such as pale skin, fatigue, rapid heart rate, and abnormal findings in the mouth (glossitis) or nails (koilonychia).
- Blood Tests:
- Blood tests are essential for confirming the diagnosis of IDA. The key blood tests used include:
- Complete Blood Count (CBC): This test measures various components of the blood, including hemoglobin, hematocrit, red blood cell count, and mean corpuscular volume (MCV). A low hemoglobin and hematocrit, along with a low MCV, suggest the presence of anemia.
- Serum Ferritin: Ferritin is a protein that stores iron in the body. Low levels of serum ferritin indicate depleted iron stores, a characteristic feature of IDA.
- Serum Iron: This test measures the amount of iron circulating in the blood. A low serum iron level can be indicative of IDA.
- Total Iron-Binding Capacity (TIBC): TIBC measures the body’s capacity to bind and transport iron. Elevated TIBC levels are often seen in IDA.
- Transferrin Saturation: This calculation (serum iron divided by TIBC) provides information about the saturation of transferrin with iron. In IDA, transferrin saturation is typically low.
- Blood tests are essential for confirming the diagnosis of IDA. The key blood tests used include:
- Additional Tests:
- In some cases, additional tests may be ordered to determine the underlying cause of iron deficiency. These tests can include stool tests for gastrointestinal bleeding, endoscopy or colonoscopy to evaluate the gastrointestinal tract, and tests for underlying medical conditions (e.g., celiac disease or inflammatory bowel disease).
- Evaluation of Response to Treatment:
- Once the diagnosis of IDA is confirmed, treatment with iron supplementation and dietary changes is initiated.
- Follow-up blood tests are conducted periodically to monitor the individual’s response to treatment and ensure that hemoglobin and iron levels are improving.
How do you educate the patient with iron deficiency anemia?
Educating a patient with iron deficiency anemia (IDA) is a crucial aspect of their overall care. Proper education helps the patient understand their condition, the treatment options, and how to make lifestyle changes to manage and potentially prevent future episodes of IDA. Here’s a step-by-step guide on how to educate a patient with iron deficiency anemia:
- Explain the Diagnosis:
- Begin by explaining the diagnosis of iron deficiency anemia. Use simple, non-medical language to ensure the patient understands the condition.
- Discuss the Causes:
- Provide information about the common causes of IDA, which may include inadequate dietary iron intake, chronic blood loss, poor iron absorption, and increased iron demands.
- Symptoms and Impact:
- Describe the typical symptoms of IDA, such as fatigue, weakness, pale skin, shortness of breath, and dizziness.
- Explain how IDA can impact the patient’s daily life, including their ability to perform tasks and activities.
- Treatment Options:
- Discuss the treatment options for IDA, including iron supplementation and dietary changes. Explain that iron supplements are available in various forms (tablets, capsules, liquid) and should be taken as prescribed.
- Emphasize the importance of following the treatment plan consistently to replenish iron stores and improve hemoglobin levels.
- Dietary Changes:
- Provide guidance on dietary changes to increase iron intake. Encourage the patient to incorporate iron-rich foods into their meals, such as lean red meat, poultry, fish, legumes, fortified cereals, dark leafy greens, nuts, and dried fruits.
- Explain the benefits of consuming vitamin C-rich foods (e.g., citrus fruits, bell peppers) with iron-rich foods, as vitamin C enhances iron absorption.
- Iron Supplements:
- Explain how to take iron supplements, including the dosage, timing, and any potential side effects (e.g., constipation, nausea).
- Emphasize the importance of not taking iron supplements with dairy products, tea, or coffee, as these can interfere with iron absorption.
- Monitoring and Follow-Up:
- Describe the need for regular follow-up appointments with a healthcare provider to monitor progress and adjust treatment as necessary.
- Discuss the importance of undergoing follow-up blood tests to track changes in hemoglobin and iron levels.
- Addressing Underlying Causes:
- If an underlying cause of IDA has been identified (e.g., gastrointestinal bleeding, heavy menstrual bleeding), explain how it will be addressed and treated.
- Preventive Measures:
- Provide information on preventive measures, such as maintaining a balanced diet rich in iron, managing underlying health conditions, and seeking medical attention for any unusual symptoms.
- Patient Questions and Concerns:
- Encourage the patient to ask questions and address any concerns they may have about their condition or treatment.
- Written Information:
- Provide written materials or resources that summarize key points about IDA, treatment, and dietary recommendations. This can serve as a reference for the patient.
- Support and Encouragement:
- Offer support and encouragement throughout the educational process. Ensure that the patient feels comfortable discussing their condition and any challenges they may encounter.
Remember that patient education is an ongoing process, and patients may need reinforcement and additional information as they manage their iron deficiency anemia. Tailor your educational approach to the patient’s individual needs and preferences, and encourage open communication to promote a collaborative and effective healthcare partnership.
Blood test for iron deficiency
Blood tests are essential for diagnosing iron deficiency and assessing the severity of the condition. Several specific blood tests can provide valuable information about a patient’s iron status. Here are the key blood tests used to diagnose iron deficiency:
- Complete Blood Count (CBC):
- A CBC measures various components of the blood, including red blood cell count, hemoglobin, hematocrit, mean corpuscular volume (MCV), and mean corpuscular hemoglobin concentration (MCHC).
- Low levels of hemoglobin and hematocrit, along with a low MCV and MCHC, are indicative of anemia, which may be caused by iron deficiency.
- Serum Ferritin:
- Ferritin is a protein that stores iron in the body. Measuring serum ferritin levels is one of the most reliable indicators of iron deficiency.
- Low serum ferritin levels suggest depleted iron stores, a characteristic feature of iron deficiency anemia.
- Serum Iron:
- A serum iron test measures the amount of iron circulating in the blood.
- Low serum iron levels can be indicative of iron deficiency, particularly when accompanied by low ferritin levels.
- Total Iron-Binding Capacity (TIBC):
- TIBC measures the body’s capacity to bind and transport iron. It reflects the availability of binding sites for iron on transferrin, a transport protein.
- Elevated TIBC levels are often seen in iron deficiency anemia.
- Transferrin Saturation:
- Transferrin saturation is calculated by dividing the serum iron level by the TIBC. It provides information about the saturation of transferrin with iron.
- In iron deficiency anemia, transferrin saturation is typically low.
- Red Blood Cell Distribution Width (RDW):
- RDW is a measure of the variation in size of red blood cells.
- In iron deficiency anemia, red blood cells may appear smaller (microcytic) and more variable in size, leading to an elevated RDW.