Based on what you have learned so far this week, create a PowerPoint presentation with detailed notes for each slide that addresses each of the following points/questions.

Assignment Description:
Professional Development Assignment
Based on what you have learned so far this week, create a PowerPoint presentation with detailed notes for each slide that addresses each of the following points/questions. Be sure to completely answer all the questions. Use clear headings that allow your professor to know which bullet you are addressing on the slides in your presentation.
Support your content with at least four (4) citations throughout your presentation. Make sure to reference the citations using the APA writing style for the presentation. Include a slide for your references at the end.
- Title Slide (1 slide)
- For a hospital to operate efficiently and effectively, the three important influences in its governance, medical staff, board of trustees, and administration, must work together in reasonable harmony. What factors contribute to the tension that usually exists among them? (4 slides).
- Organizations such as the LeapFrog Group represent a growing trend to survey and report on the quality of hospital care and to make the findings available to the public. What are your opinions about the public’s readiness to deal with having this information available and using it to make choices about medical care? (2-3 slides)
- Hospitals are facing unprecedented financial challenges from entrepreneurial physician initiatives that are establishing competitive, free-standing diagnostic and treatment centers and specialty hospitals. What are the advantages and disadvantages to these developments from a patient perspective? (2-3 slides)
- References (1 slide)
Expert Answer and Explanation
Every organization has its own power structure that influences different dynamics which shape the culture of the organization. Three major influencing forces, namely the governance, medical staff, board of trustees, and administration at times engage in conflicting situations that are likely to cause tensions. Some of the causes that bring about these tensions include the following;
- Conflicting interests – This usually occurs when each wing has a conflicting goal with the other. In most cases, it is supposed to be the organization’s leadership that brings unity of purpose steered towards achieving organizational goals. However, without the alignment of goals among the different entities, then there is likely to be tension (Antonacci et al., 2018).
- Resource allocation – Resources are usually scarce. When the medial staff are not accorded the required resources to execute their mandate there is a high likelihood for tensions to occur across the different entities.
- Communication breakdown – Poor communication is always a recipe for organizational conflicts. When instructions are not understood, or when a party is kept in the dark concerning the going-on of the organizations, there is likely to be build-up of tension.
- Performance expectations – Failure to meet the targets agreed upon can also cause tensions to exist. There are times when unrealistic targets are set for the medical staff, for example, targets that conflict with the business perspective of the facility. Such targets can be a source of demotivation leading to tension between the different groups (Labelle et al., 2016)
- Organizational change – Unplanned change can cause significant resistance to exist from any of the influential groups.
- Existing allegiances and power struggles – Power dynamics within the organization, including how reward and punishment is delivered can cause tension. Tendency to be biased when making important decisions favoring a particular cluster of people within the organization brig about discontentment leading to build-up of tension.
(Figueroa et al., 2019)

- Failure to respond to existing issues – There are time when the administration or the board fails to approve or deal with pertinent issue concerning medial staff for example approving additional staff to be employed. This can lead to conflict between the different influences.
- Lack of accountability – Transparency is crucial in the management of organizational operations. In an environment where no one is brought to account for expenditure, operational efficiency, leadership, or general organizational performance, tensions are bound to exist (Figueroa et al., 2019).
Publication of data plays a critical role in improvement of the standards of care quality. Care facilities depend on the data collected from independent entities to improve their internal systems allowing provision of superior care in terms of quality and safety. The following are some of the reasons why healthcare facilities should encourage publication of findings by independent organizations.
- Data allows provision of enhanced quality of care
- Implementation of evidence-based practice
- Creation of innovative practices in clinical practice
- Foundation of new frontiers in research (Hagan et al., 2017)
- Enhanced health literacy=- Over time, the level of patients, health literacy has been goring making them more aware of their health needs and outcomes.
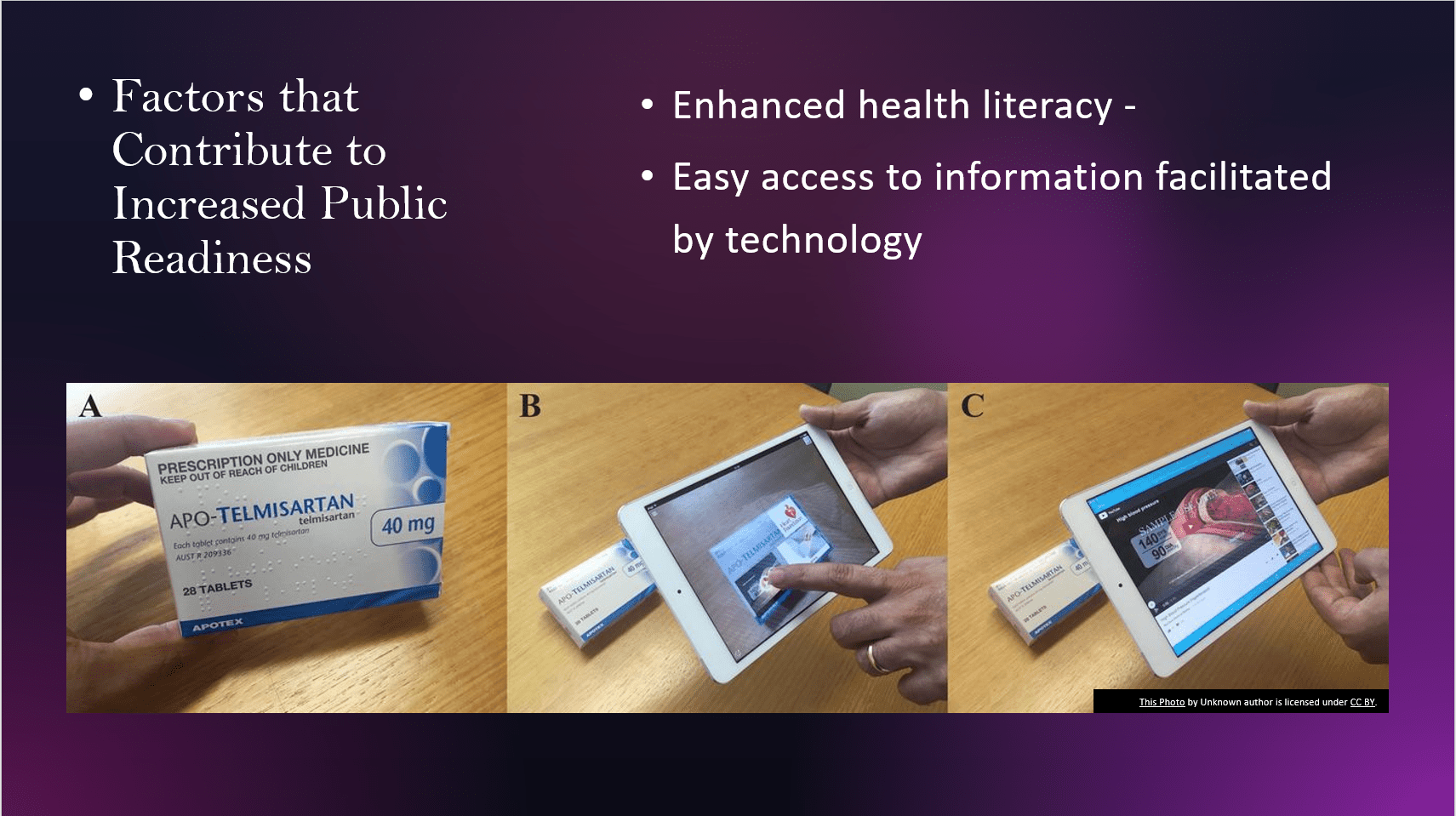
- Easy access to information facilitated by technology – Technology has made access to information easy. Using technology, patients can easily access information which at times influence their decision making when it comes to health preferences.
- Increased sensitization on patients’ right to quality and safe care – After the enactment of the ACA, there have been increased efforts to sensitize patients about the provision of quality care
- Increased call to provide patient-centered care – Similarly, in conformance with the value-based system, there has been increased involvement of patients in clinical decision making which has contributed to increased appetite to consume healthcare information.
Specialty facilities are those that have a limited range of services, providing specialized therapeutic and diagnostic services addressing specific patient needs (Sultz & Young, 2017). There are several factors that have given rise to specialty hospitals. Some of them include
- Increased advancements in healthcare, especially technological advancements.
- Increased competition within the healthcare industry
- Changes in patient demands and the need for quality care
- Changes in population dynamics, for example the increasing baby boomer generation has seen a growth in long-term care facilities.
- Focused experience from healthcare personnel thus improved quality of care – Staff working in specialty hospitals are usually trained and have the experience to handle patients with a specific condition making their interventions more targeted and refined which usually equates to better quality.
- Specialized resources for targeted patient groups – Specialty hospitals provide targeted resources and programs that are specific to targeted patient groups which increase the level of efficacy in addressing patient needs (Sultz & Young, 2017)
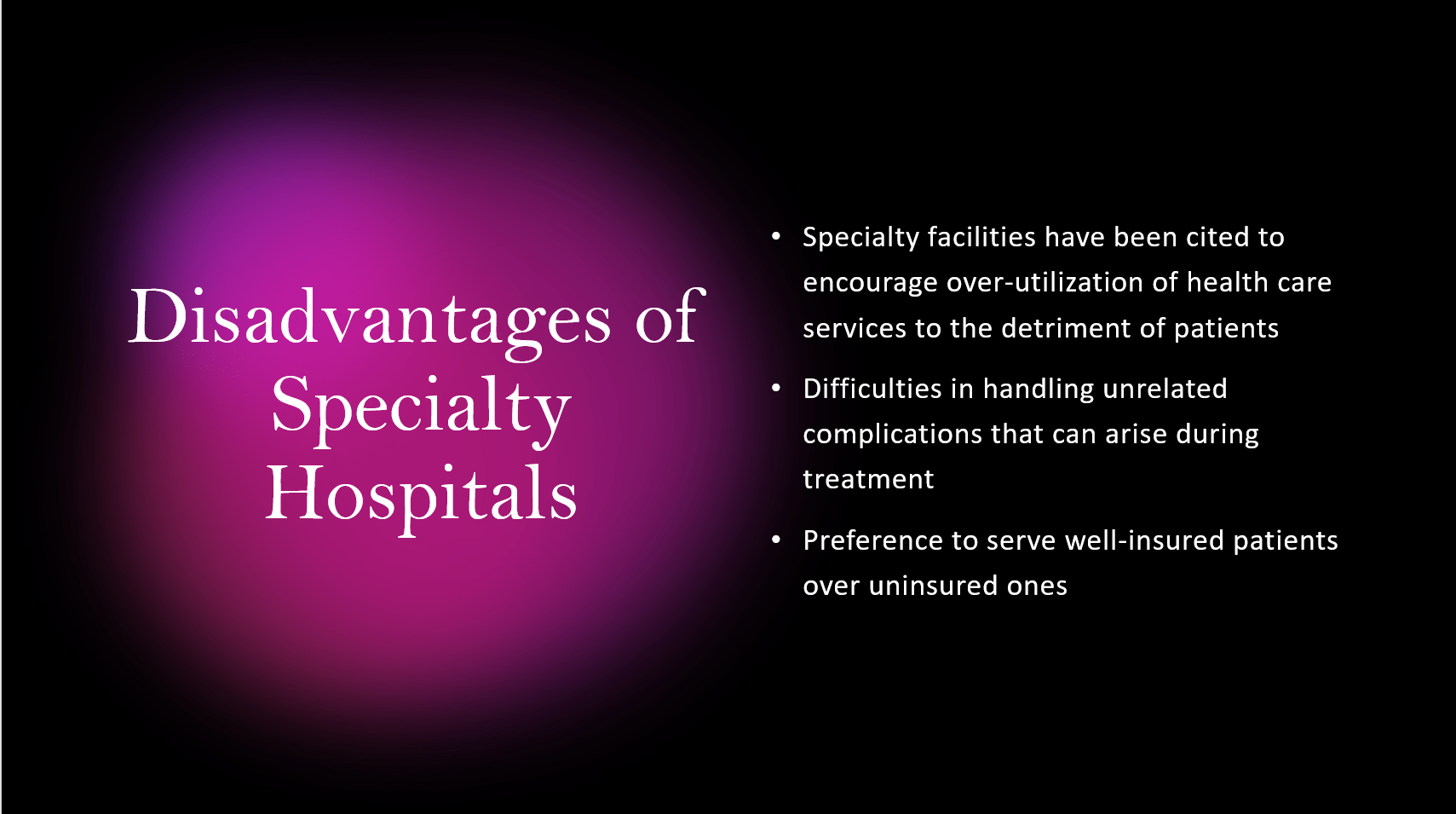
- Specialty facilities have been cited to encourage over-utilization of health care services to the detriment of patients, more so due to collusions or conflicting interests that tend to increase referrals to such facilities that are mostly owned by physicians.
- Difficulties in handling unrelated complications that can arise during treatment – This is especially true given the dynamic nature of clinical environment where one condition can likely trigger another that is not treated in the specialty facility.
- Preference to serve well-insured patients over uninsured ones which increases the level of disparity in healthcare.
References
Antonacci, G., Reed, J. E., Lennox, L., & Barlow, J. (2018). The use of process mapping in healthcare quality improvement projects. Health services management research, 31(2), 74-84.
Figueroa, C. A., Harrison, R., Chauhan, A., & Meyer, L. (2019). Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC health services research, 19(1), 1-11.
Hagan, T. L., Schmidt, K., Ackison, G. R., Murphy, M., & Jones, J. R. (2017). Not the last word: dissemination strategies for patient-centred research in nursing. Journal of research in nursing : JRN, 22(5), 388–402. https://doi.org/10.1177/1744987117709516
Labelle, F., De Rouffignac, A., Lemire, P. O., Bredillet, C., & Barnabé, S. (2016). Managing tensions and paradoxes between stakeholders in a complex project context: Case study and model proposal. Journal of Modern Project Management, 7(2), 247-275.
Sultz, H. A., & Young, K. A. (2017). Health care USA: Understanding its organization and delivery(9th ed.). Jones & Bartlett.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon: NEW30 to Get 30% OFF Your First Order
Use Coupon: NEW30 to Get 30% OFF Your First Order

Other Assignment Questions Related to this Class:
Module 1 Discussion Question:
The practice of medicine, long valued for individual entrepreneurship and physician control, has undergone dramatic change. Physicians now face vexing oversight of case and utilization management and loss of control over the allocation of health care dollars. Managed care organizations control health costs by arbitrarily refusing reimbursement for certain medical procedures and reducing payments for others. Since medicine is now a less attractive career option, will fewer high performing individuals choose to become physicians? What are the implications for the quality of care?
Module 1 Assignment
Assignment Description:
Complete ALL of the bullet points below:
- Health care planners could be more effective and efficient if they used the concept of the natural history of disease and the levels of prevention to design services that intervene at the weakest link in the chain of progression of specific diseases. Instead, most focus on high-technology solutions to preventable problems. Assess the characteristics of the medical care culture that encourage the latter approach.
- Hospitals and other health care institutions, whether voluntary or for-profit, need to be financially solvent to survive growing market pressures. Describe how this “bottom line” focus has changed the nature of the US health care system.
- The insurance industry plays a huge role in the American health care system and absorbs a significant portion of the health care dollar. A single payer system, whether it is a private company or the US government, would eliminate the complex insurance paperwork burden and free substantial funds that could be diverted to support care for the under-served. Why do you believe that so much resistance to a concept used in every other developed country has continued in the U.S.?
- Include the time management Weekly Planner to show when you will make room for your school work.
Please submit one APA formatted paper between 1000 – 1500 words, not including the title and reference page. The assignment should have a minimum of two scholarly sources, in addition to the textbook.
Module 2 Discussion Question:
Considering significant issues with availability of hospital beds in the United States, what is the rationale for taxpayer support of the separate hospital system of the Department of Veterans Affairs?
Module 3 Discussion Question:
Hospital emergency departments continue to be used as a source of primary medical care by large numbers of the community’s medically underserved population. What are the implications of this practice for the patients, and on health care costs and quality of care? What would you propose as a means to change this situation?
Module 3 Assignment
Assignment Description:
Complete ALL of the bullet points below:
- Given the increasing longevity of Americans and the costs of providing long-term care, anticipation of the costs should be a major element of every family’s financial planning. Current information suggests however, that very few families or individuals give this consideration. What factors might impede this advance planning? What measures might be effective in raising awareness among Americans about this important matter?
- Identify the major factors that have resulted in the shift in utilization from inpatient hospitalization to ambulatory care services. What are the implications of this shift for hospitals, consumers, and the health care delivery system as a whole?
- The recipients of mental health services in the US represent only a small percentage of those in need of services. Discuss the factors that impede access to mental illness treatment.
- Include a screenshot of your note taking from your reading this week.
Please submit one APA formatted paper between 1000 – 1500 words, not including the title and reference page. The assignment should have a minimum of two (2) scholarly sources, in addition to the textbook.
Module 4 Discussion Question:
In 1992, medical residency programs in the U.S. were described as “responsive principally to the service needs of hospitals, the interests of the medical specialty societies, the objectives of the residency program directors, and the career preferences of the medical students.” In fact, there are so many more residency programs than can be filled by American medical school graduates, that an annual influx of foreign educated physicians has been required to satisfy the service needs of many hospitals.
In addition, until recently, there has been no attempt to match America’s needs for various kinds of specialty and generalist physicians with the hospital-based training programs that were producing them. In light of these facts, pose an opinion on this question:
Few graduates of medical school choose primary care, and instead flock to specialties with greater pay and prestige. Since primary care is the basis for maintaining health and early diagnosis of potential health problems, who should be responsible for rectifying this misplaced emphasis of health care, insurers, medical schools, the government, the AMA, and others?
Module 4 Assignment Description
Professional Development Assignment:
Based on what you have learned so far this week, create an educational presentation with detailed notes and recorded audio comments for all content slides that addresses each of the following points/questions. Be sure to completely answer all the questions. Use clear headings that allow your professor to know which bullet you are addressing on the slides in your presentation.
Support your content with at least four (4) citations throughout your presentation. Make sure to reference the citations using the APA writing style for the presentation. Include a slide for your references at the end. Follow best practices for PowerPoint presentations (an example is located in the Resources tab) related to text size, color, images, effects, wordiness, and multimedia enhancements. Use the audio recording feature with the PowerPoint. Alternatively, you may use a smartphone or tablet to record yourself speaking, should you be unable to use the audio feature within PowerPoint.
- Title Slide (1 slide)
- The various kinds of health professionals are educated in separate schools but with considerable overlap in curricula and training requirements. They are, however, expected to integrate their training and work together after graduation. Identify the advantages and disadvantages of this approach to professional education in terms of costs, educational efficiency, and patient care quality. (4 slides)
- An oversupply of physicians in many urban regions contrasts with continuing problems of access in rural and inner-city areas. Why does the mal-distribution of physicians persist in spite of the number of physicians graduated? (2-3 slides)
- The health care delivery system now places increased emphasis on maintaining wellness and on promoting disease avoidance through healthy behaviors and lifestyles. What challenges does this new orientation pose for our existing system of medical education and training? (2-3 slides)
- References (1 slide)
Module 5 Discussion Question:
Many consumer and health care advocacy initiatives are converging toward a mandate to provide public access to many types of information about managed care organization (MCO) performance, costs, and quality. In fact, employers in the many parts of the country who are the major purchasers of health insurance are now requiring MCOs to make “health plan performance data” available to subscribers to facilitate their choice of plans.
Discuss and provide the rationale for your opinion on providing data in areas such as patient outcomes, compliance with national standards for preventive and chronic care, and comparative costs to the public.
What obligation, if any, does an employer, and/or MCO have to educate subscribers in how to interpret performance data? At whose expense should such education be provided?
What are the possible benefits or disadvantages to making such performance data available to the public?
Module 5 Assignment
Assignment Description:
Complete ALL of the bullet points below:
Compare and contrast each of the three questions related to Managed Care Organizations, Medicare, and Medicaid with one another and explain how they were similar and different to each other.
- Managed care organizations emphasize physicians’ responsibilities to control patient access to expensive hospitalization and specialty care, a principle dubbed “gatekeeping.” Some argue that “gatekeeping” is unethical because it introduces financial factors into treatment decisions. Others say it improves quality by promoting the use of the most appropriate levels of care.
- Medicare is an area that often gets overlooked and is seen as a burden financially. Discuss alternatives to ease the drain on Medicare resources.
- Medicaid is shouldering an ever-increasing burden of cost for long-term care for the elderly, with enormous impacts on state budgets throughout the nation. Discuss alternatives to ease this drain on Medicaid resources.
Develop an APA-formatted essay discussing the three entities.
Describe what they are and how they differ. Include an introduction to let the reader know what will be found in the essay.
Create a table to provide comparison of the three entities. The table can be used as the body of the paper, or it can be added as an addendum after the Reference page. If you opt to add it as an addendum, refer to the table in the narrative in the body of the essay.
As in all essays, include a conclusion to provide a summary of the material. This assignment highlights your ability to do research and display information in a table format. Include citations, as appropriate, for information in the table. Refer to chapter 7 in the APA manual, specifically pages 223 -224 for information on tables using words for displaying information.
Module 6 Discussion Question:
It is unfortunate that it requires a threat, epidemic, or pandemic to halt the demise of organized public health and restore an effective public health structure. Why does public health have so much difficulty maintaining governmental support of its central role in maintaining the health and well-being of the American people?
Module 6 Assignment
Assignment Description:
Professional Development Assignments:
- Public health efforts and those of private medicine complement each other and together serve the spectrum of health service needs of American society. Why, then, has their relationship been so contentious?
- The Institute of Medicine report of 1999 cites two major studies that establish medical errors as one of the leading causes of death and disability in the United States. Should the federal government take the necessary steps to monitor the status of this high-risk situation, as it does with other epidemics, or should the government continue to trust the providers of health care to deal forthrightly with the problem?
- Analyze why legislative attempts to address only one of the trio of rising costs, lack of universal access, or variable quality of health care only worsens the remaining two.
Please submit one APA formatted paper between 1000 – 1500 words, not including the title and reference page. The assignment should have a minimum of two (2) scholarly sources, in addition to the textbook.
Module 7 Discussion Question:
For many years, hospital accreditation bodies assumed that if the structural criteria were met, that is, that the physical plant, the qualifications of the staff, and the necessary equipment were in place, the quality of the services would automatically be acceptable. Subsequently, accreditation groups decided that they had also better look at the medical records to see how the services were being provided. They assumed that, if the necessary structure was in place, and the required services were delivered as prescribed, the quality of care would be acceptable. Now, these same accrediting groups find it necessary to look at the outcomes of care as well.
Describe “structure, process, and outcome” in the assessment of the quality of medical care, and provide examples of each dimension.
How are the three dimensions related?
Can these relationships be trusted to assure the quality of care in the complex, high-tech world of modern medicine? If not, why?
Module 7 Assignment
Assignment Description:
Complete ALL of the bullet points below:
• Definitions of the quality of medical care are no longer left to clinicians who decide for themselves what technical performance constitutes “good care.” What are the other dimensions of quality care and why are they important? What has changed since the days when “doctor knows best?”
• Quality in medical care may be defined as achieving the greatest benefit at the lowest risk. How have the priorities of our health care system and the allocation of resources addressed this goal?
• Contrast the definitions of implicit and explicit criteria in assessing health care quality. How is each type of criterion useful in quality assessment?
Please submit one APA formatted paper between 1000 – 1500 words, not including the title and reference page. The assignment should have a minimum of two (2) scholarly sources, in addition to the textbook.
Module 8 Discussion Question:
The wisdom of depending on International Medical School Graduates (IMGs) to fill gaps in physician supply, while US medical schools hold class size constant, is questionable. In addition, the aging of the physician workforce, the decreasing hours worked by both physicians in practice and physicians in residency, and a 20 percent reduction in the effort of the increasing proportion of minority physicians, will result in a significant decrease in the “effective” supply of physicians. Should the gap be filled by a major substitution of nurse practitioners, physician assistants, chiropractors, acupuncturists, and others, or are there alternatives?
Module 8 Assignment
Assignment Description:
Signature Assignment: Improving Health Care Delivery
Presentation:
Among various stakeholders, the registered nurse is an advocate for patients, their health and the care delivered to them. There is a need to evaluate the health status of vulnerable populations, to assess nursing’s role in health initiatives, and to find ways that we can help improve health. This presentation enables students to assess the role of organized efforts to influence health care delivery, and the contributions of medical technology, research findings, and societal values on our evolving health care delivery system.
This presentation will examine the role of the nurse as a health professional and leader.
• Choose a high-risk risk population
• Address a health care need for this population
• What resources are provided for this population?
• What are the economic priorities, challenges, and issues for this population?
• What are the major ethical, societal, professional, and legal system-level issues confronting providers, insurers, public policymakers, and organizations regarding the care for this population?
• How could nursing intervene or advocate to improve the health care delivery for this population?
Total Point Value of Signature Assignment: 400 points
FAQs
What are the three components of hospital governance?
Hospital governance typically involves three main components:
- Board of Directors: The board of directors is a group of individuals responsible for overseeing the hospital’s overall strategy, policies, and performance. Members of the board are often selected based on their expertise in areas such as healthcare, finance, law, and management. They play a crucial role in decision-making and ensuring the hospital’s adherence to its mission and values.
- Executive Leadership Team: The executive leadership team consists of senior management officials, including the Chief Executive Officer (CEO), Chief Medical Officer (CMO), Chief Financial Officer (CFO), and other key executives. This team is responsible for the day-to-day operations of the hospital and implementing the strategic direction set by the board. They also manage the hospital’s financial health, quality of care, and overall organizational performance.
- Medical Staff and Clinical Leadership: The medical staff, including physicians and other healthcare professionals, contribute to the governance structure by participating in decision-making processes related to clinical policies, patient care, and quality improvement. Clinical leaders, such as the Chief Medical Officer, work closely with the executive leadership team to ensure that medical and clinical practices align with the hospital’s goals and regulatory standards.
These three components work together to establish a governance framework that promotes effective leadership, accountability, and the delivery of high-quality healthcare services.
What are the five major responsibilities of a governing board?
The governing board of a hospital typically has five major responsibilities:
- Strategic Direction and Planning: The board is responsible for setting the hospital’s overall strategic direction. This involves defining the mission, vision, and values, as well as establishing long-term goals and objectives. The board works collaboratively with the executive leadership team to develop strategic plans that guide the organization in achieving its mission.
- Policy Development and Oversight: Governing boards are tasked with developing and approving policies that govern the operation of the hospital. These policies cover a wide range of areas, including patient care, safety, financial management, and compliance with regulations. The board ensures that policies are in line with legal requirements and best practices.
- Financial Oversight: The board is responsible for ensuring the hospital’s financial health. This includes approving budgets, monitoring financial performance, and overseeing financial policies. Boards work closely with the finance committee and executive leadership to make informed decisions about resource allocation and financial sustainability.
- Quality and Patient Safety Oversight: Ensuring the delivery of high-quality healthcare services and maintaining patient safety are critical responsibilities of the governing board. Boards monitor quality metrics, patient satisfaction, and safety initiatives. They collaborate with the executive leadership team to implement continuous improvement processes and address any issues related to patient care quality.
- CEO Selection and Performance Evaluation: The board is involved in the selection, appointment, and evaluation of the Chief Executive Officer (CEO). Selecting the right CEO is crucial for the success of the hospital, and the board assesses the CEO’s performance against established goals and expectations. The board also provides guidance and support to the CEO in their leadership role.
What are the duties of the governing board in a hospital?
The duties of a governing board in a hospital encompass a range of responsibilities to ensure effective governance, strategic direction, and the delivery of high-quality healthcare services. Here are key duties of a hospital governing board:
- Setting Strategic Direction:
- Define and articulate the hospital’s mission, vision, and values.
- Establish long-term strategic goals and objectives.
- Provide guidance on major organizational initiatives and priorities.
- Policy Development and Oversight:
- Develop and approve policies that govern the hospital’s operations.
- Ensure policies align with legal requirements, ethical standards, and best practices.
- Monitor and evaluate the implementation of policies.
- Financial Oversight:
- Approve and oversee the hospital’s budget.
- Monitor financial performance and ensure fiscal responsibility.
- Review and approve major financial decisions and investments.
- Address financial challenges and work toward sustainability.
- Quality and Patient Safety Oversight:
- Monitor and assess the quality of healthcare services provided by the hospital.
- Implement systems to ensure patient safety and prevent medical errors.
- Review and address issues related to patient care quality.
- Collaborate with the executive leadership team on quality improvement initiatives.
- CEO Selection and Performance Evaluation:
- Participate in the selection and appointment of the Chief Executive Officer (CEO).
- Establish performance expectations for the CEO.
- Regularly evaluate the CEO’s performance against established goals.
- Provide guidance and support to the CEO in their leadership role.
- Community and Stakeholder Engagement:
- Foster positive relationships with the community, patients, and other stakeholders.
- Communicate transparently with the public and stakeholders about the hospital’s activities and performance.
- Seek and consider input from various stakeholders.
- Compliance and Legal Oversight:
- Ensure compliance with relevant laws, regulations, and accreditation standards.
- Address legal and regulatory matters affecting the hospital.
- Implement effective risk management strategies.
- Advocacy and Representation:
- Advocate for the hospital and its mission in the broader community.
- Represent the hospital’s interests to government agencies, policymakers, and other organizations.
- Ethical Decision-Making:
- Uphold high ethical standards in all aspects of hospital governance.
- Make ethical decisions in the best interests of patients and the community.
- Continuous Improvement:
- Regularly assess the effectiveness of the governing board’s own performance.
- Engage in ongoing education to stay informed about healthcare trends, challenges, and best practices.
- Implement changes and improvements to enhance the governance structure.
