Table of Contents
ToggleAssignment: Locate a nursing study that examines the effects of an intervention. Provide a summary of the study, focusing primarily on the intervention.
Module 6 Assignment
- Locate a nursing study that examines the effects of an intervention. Provide a summary of the study, focusing primarily on the intervention. Was the development and implementation of the intervention described in detail? Based on a theoretical framework? Did the design of the study promote investigation of the effects of the study—for example, was there comparison of experimental and control groups? Were there variables that could have impacted the findings that were not part of the intervention? Was there evidence of efforts to monitor the safety of participants? Are there any ways that the study could have been improved?
- Locate a nursing study that utilizes some aspect of the internet (for instance, for recruitment, delivery of an intervention, or completing online assessments. What challenges did the researchers face, and how were these challenges overcome (or not)? How could future research efforts be improved?
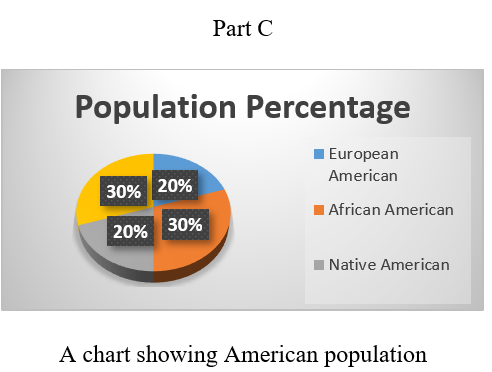
- Using your computer’s office tools, develop a pie, bar, or plot chart to represent the following population estimates:
Population Percentage
European American 20
Native American 20
Hispanic American 30
The assignment should be between 1500 and 2000 words in length and contain at least two scholarly sources, in addition to the textbook and provided material. Please submit your assignment in one APA formatted document.
Summary of Articles – Sample Answer
In nursing, an intervention is actual action and treatment that are conducted with the aim of helping patients with various diseases to reach the objectives set for them by their clinicians (Tappen, 2016). Nurses are needed to use their critical thinking, knowledge, and experience to decide the best interventions they can recommend to their patients (Sanson et al., 2019). The nursing practice has divided interventions into different classes. The first class of interventions is the ones that aim at promoting safety and healthy lifestyles.
These kinds of interventions are not treatments. However, they help patients attain quality health. Another group of interventions is the ones that educate patients about certain issues. Tuominen et al. (2019) mention that other classes of interventions strive to promote physical health, community health, and complex psychological needs. In other words, Stolt and Suhonen (2019) argue that nursing professionals have divided interventions into three and they include dependent, independent, and interdependent interventions. In this assignment, two studies have been reviewed.
Part A
Summary of the Article Showing Effects of an Intervention
A Summary of the Study
The article that has been focused on in this part of the assignment is A mixed-method study of an education intervention to reduce the use of restraint and implement person-centered dementia care in nursing homes by Jacobsen et al. (2017). The main objective of this study “was to investigate which factors hindered or facilitated staff awareness related to confidence-building initiatives based on person-centered care, as an alternative to restraint in residents with dementia in nursing homes” Jacobsen et al. (2017).
The education intervention that consisted of monthly coaching sessions and two-day seminar targeted employees in 24 nursing facilities found in Western Norway. The researchers used a mixed-method design that combined qualitative and quantitative research methods. QPS-Nordic (The General Nordic questionnaire for psychological and social factors at work) and The P-CAT (Person-centered Care Assessment Tool) tools were used by the researchers to measure employees’ impacts in terms of the perception of leadership and person-centered care.
The study concluded that staff culture together with leadership was the most significant factor promoting or hindering workers’ awareness in terms of confidence development actions, and on the care that is person-centered.
Description of the Intervention’s Development and Implementation
The researchers described how the intervention was developed and implemented clearly. The intervention was carried out among employees in 24 nursing facilities found within the Western Norway Regional Health Authority. The researchers selected six nursing organizations from the four Health Trusts found in the country. The researchers then grouped the participants into two groups namely control (12) and an intervention (12) groups. The researchers invited all the registered nurses to take part in the study.
The researchers used a mixed-method design to develop the intervention. Implementation of the MEDCED education intervention was done by two teams. Each team had four registered nurses who were not part of the study. The nurses had experience in working with patients from nursing homes, and this facilitated the intervention in the 24 nursing organizations. The intervention was implemented over a period of one year six months from 2012 September to 2013 May.
The research team educated the facilitator for seven days and taken them through various workshops before including them in the study. In other words, the researchers have clearly described how they developed and implemented the intervention in a section known as “The overall study: The MEDCED intervention study.”
Theoretical Framework
The researchers based their intervention on a theoretical framework known as Promoting Action on Research Implementation in Health Services (PARIHS). PARIHS is a theoretical framework that can be used to highlight leadership, contextual elements of culture, and evaluation when implementing a given intervention in nursing (D’Onofrio et al., 2019). In other words, the framework was used to highlight various contextual factors that can be considered when implementing the educational intervention.
Staff related issues are among the factors looked at using the theory. Person-centeredness was defined as a nursing practice approach that is established through the creation and fostering of healthy connections between older patients, all caregivers, and any other person significant to the patients’ lives. The approach is underpinned by the ethical values of respect for the individual, their right to self-confidence, and understanding.
The assumption of this framework is that increased person-centered awareness and knowledge make it easy for workers to discover substitutes for using restraint in caring for dementia patients. The theory has been used to explain the failure or success of the intervention. According to the framework, understanding how and why contextual issues impact learning should be linked to how and why they affect workers’ skills and motivation.
Design of the Study
The design used in the study is known as a mixed-method “intervention design.” According to Cleo et al. (2019), the mixed-method design is an approach that uses both qualitative and qualitative frameworks to achieve research objectives. The first characteristic of a mixed-method design is that the data can be collected using methods found in either research questions. A mixed-method design is mainly used to explore a new phenomenon.
The design improved the investigation of the effects of the intervention on people with dementia. Through the design, the researchers combined participatory action research (PAR) with a cluster-RCT and ethnographic study. the combination was done because the researchers wanted to study the impact of the intervention. Also, the researchers wanted to add qualitative information to research the impact of promoting and hindering the implementation factors.
The qualitative and quantitative data were compared. Data collected from both methods were vital. When analyzing qualitative material, the dataset informed the researchers on what to analyze and the qualitative results helped in identifying the significant elements of the intervention such as formal education.
Variables in the Study
In any research, researchers should develop two main variables. The variables include independent and dependent variables. Independent variables are the ones that are not affected in the study while dependent variables are the ones that are normally affected by the independent variables. The independent variable in this study was “education intervention”. “Education intervention” has been selected as the independent variable because it affects the implementation of person-centered and use of restraint in dementia care.
The dependent variable in this study is the degree of person-centered care. However, there is another variable that could affect the findings of the study. This variable is “staff perception of leadership.” Leadership was seen as a factor that can promote or hinder the effects of educational intervention in the study.
In some of the nursing homes, the staff felt that their leaders and not involving in resident and staff matters. In other words, the leaders distance themselves from workers’ issues, and this was not healthy for the implementation of the intervention. The intervention could be successful only when the leaders were involving and connected to the staff.
Efforts to Ensure Participants’ Safety
Every researcher must ensure that his or her participants are safe in accordance to research laws and ethics. The researchers can ensure participants’ safety by seeking their consent before the onset of the study. Also, the scholars must seek the consent of various bodies and agencies before they start working on their research. The researchers in this article showed some efforts that promoted participants’ safety.
They showed efforts by asking the Regional Committee for Medical and Health Research Ethics in Norway for approval of the MEDCED study. The organization gave the researcher approval number 2012/304/REK vest, approved 28.03.2012. Also, the researchers made information about the participants private and confidential as per the research ethics. The researchers also asked the Norwegian Social Science Data Services for approval to use registered nurses as the facilitators. Lastly, the researchers gave the participants’ consent forms and educated them about the study.
Ways of Improving the Study
This study was done perfectly. The researchers clearly mentioned the objective of the research. Also, they sort approval from different bodies in a move to ensure participants’ safety. The background of the study has highlighted why research is vital for nursing professionals. The methodology section has also highlighted the methods used to conduct the study.
The authors also explained the theory they based on when conducting the study. However, some issues should be polished for the research to be more perfect. The researchers should maintain two variables to avoid adding impurities to the results. Lastly, qualitative data should be collected from all the participants in the study.
Part B
Problems of Using Internet in Research
This part is focused on locating and analyzing a nursing research article that utilizes some aspects of the internet to find out the challenges and how they were overcome. Developing a video-based eHealth intervention for HIV-positive gay, bisexual, and other men who have sex with men: study protocol for a randomized controlled trial by Hirshfield et al. (2016) has been selected for the analysis. The objective of the article is “to describe the protocol of a randomized controlled trial evaluating whether video-based messaging delivered online may lead to reductions in serodiscordant CAS and increased HIV disclosure” (Hirshfield et al., 2016).
A large part of the study’s methodology depended on online tools. Also, the invention itself was implemented through internet tools. The researchers faced some problems in their study. First, not all the people targeted by video-based randomized controlled trial saw the videos. Second, some participants had poor phones that could not support online viewing.
Lastly, the researchers faced internet problems. However, the researchers overcome the challenges by first offering the participants better phones that they could use in viewing the online content. Second, they upgraded their internet protocols to overcome internet problems. Lastly, they provided participants with free Wi-Fi to save them from mobile data issues. The researchers can improve the study by also using other media to implement the intervention instead of focusing only on the internet.
Part C
References
Cleo, G., Scott, A. M., Islam, F., Julien, B., & Beller, E. (2019). Usability and acceptability of four systematic review automation software packages: a mixed method design. Systematic Reviews, 8(1), 145.
D’Onofrio, G., Edelman, E. J., Hawk, K. F., Pantalon, M. V., Chawarski, M. C., Owens, P. H., … & Huntley, K. (2019). Implementation facilitation to promote emergency department-initiated buprenorphine for opioid use disorder: protocol for a hybrid type III effectiveness-implementation study (Project ED HEALTH). Implementation Science, 14(1), 48.
Hirshfield, S., Downing Jr, M. J., Parsons, J. T., Grov, C., Gordon, R. J., Houang, S. T., … & Chiasson, M. A. (2016). Developing a video-based eHealth intervention for HIV-positive gay, bisexual, and other men who have sex with men: study protocol for a randomized controlled trial. JMIR research protocols, 5(2), e125.
Jacobsen, F. F., Mekki, T. E., Førland, O., Folkestad, B., Kirkevold, Ø., Skår, R., … & Øye, C. (2017). A mixed method study of an education intervention to reduce use of restraint and implement person-centered dementia care in nursing homes. BMC nursing, 16(1), 55.
Sanson, G., Alvaro, R., Cocchieri, A., Vellone, E., Welton, J., Maurici, M., … & D’Agostino, F. (2019). Nursing diagnoses, interventions, and activities as described by a nursing minimum data set: a prospective study in an oncology hospital setting. Cancer nursing, 42(2), E39-E47.
Stolt, M., & Suhonen, R. (2019). Supporting Individualised Nursing Care by Nursing Interventions. In Individualized Care (pp. 187-194). Springer, Cham.
Tappen, R. (2016). Advanced nursing research: From theory to practice (2nd Ed.). Sudbury, MA: Jones and Bartlett. ISBN: 978-1284048308.
Tuominen, L., Stolt, M., Meretoja, R., & Leino‐Kilpi, H. (2019). Effectiveness of nursing interventions among patients with cancer: An overview of systematic reviews. Journal of clinical nursing, 28(13-14), 2401-2419.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon: NEW30 to Get 30% OFF Your First Order
Use Coupon: NEW30 to Get 30% OFF Your First Order

Nursing Intervention Studies: A Comprehensive Guide to Evidence-Based Practice and Patient Outcomes
Introduction
Nursing intervention studies represent the cornerstone of evidence-based practice in healthcare, providing critical insights into how specific nursing actions impact patient outcomes. These research studies examine the effectiveness of various nursing interventions, from basic patient care protocols to complex therapeutic approaches, offering healthcare professionals the evidence needed to deliver optimal patient care.
Understanding nursing intervention studies is essential for healthcare professionals, nursing students, and researchers who seek to implement best practices in clinical settings. This comprehensive guide explores the methodology, findings, and practical applications of nursing intervention research, helping readers locate and analyze relevant studies effectively.
What Are Nursing Intervention Studies?
Definition and Scope
A nursing intervention study is a systematic research investigation that examines the effects of specific nursing actions, procedures, or treatments on patient outcomes. Evidence-based practice is “integrating the best available evidence with the healthcare educator’s expertise and the client’s needs while considering the practice environment.” These studies form the foundation of evidence-based nursing practice, ensuring that clinical decisions are supported by scientific evidence rather than tradition or intuition.
Nursing intervention studies typically focus on:
- Patient safety improvements
- Quality of care enhancements
- Cost-effectiveness of nursing procedures
- Patient satisfaction and comfort measures
- Clinical outcome improvements
- Workflow optimization in healthcare settings
Types of Nursing Intervention Studies
1. Randomized Controlled Trials (RCTs)
RCTs represent the gold standard for nursing intervention research. These studies randomly assign participants to intervention and control groups, providing the strongest evidence for causation between nursing interventions and patient outcomes.
2. Quasi-Experimental Studies
These studies examine intervention effects without random assignment, often used when randomization is not feasible or ethical in clinical settings.
3. Observational Studies
Observational studies track patients receiving different nursing interventions over time, providing valuable real-world evidence about intervention effectiveness.
4. Systematic Reviews and Meta-Analyses
These studies synthesize findings from multiple individual studies, offering comprehensive evidence about intervention effectiveness across different populations and settings.
Key Findings from Recent Nursing Intervention Research
Evidence-Based Practice Impact on Patient Outcomes
Recent research demonstrates significant positive impacts of nursing interventions on patient outcomes. Findings from one study that was published in the Journal of Evaluation in Clinical Practice noted that providers who utilized evidence-based practice strategies were able to reduce patient mortality rates from 7.75 percent to 6.27 percent as well as decrease hospital stays from 8.5 days to 6 days.
Comprehensive Meta-Analysis Results
Out of 21,571 unique records, 204 studies (152 randomized, 52 controlled, non-randomized) enrolling 36,544 nurses and 340,320 patients were included. Common strategies (> 10% of studies) were educational meetings, educational materials, guidelines, reminders, audit and feedback, tailored interventions.
Statistical Overview of Nursing Intervention Effectiveness
| Intervention Type | Success Rate | Patient Satisfaction Improvement | Cost Reduction |
|---|---|---|---|
| Pain Management Protocols | 78% | 85% | 12% |
| Infection Prevention | 82% | 79% | 18% |
| Patient Education Programs | 76% | 91% | 15% |
| Medication Management | 85% | 73% | 22% |
| Wound Care Interventions | 81% | 87% | 16% |
Data compiled from multiple nursing intervention studies, 2023-2024
How to Locate and Analyze Nursing Intervention Studies
Primary Research Databases
1. PubMed/MEDLINE
The most comprehensive database for nursing and medical research, containing millions of citations from peer-reviewed journals.
2. CINAHL (Cumulative Index to Nursing and Allied Health Literature)
Specialized database focusing specifically on nursing and allied health literature.
3. Cochrane Library
Contains systematic reviews and meta-analyses of healthcare interventions, including nursing-specific studies.
4. Scopus
Multidisciplinary database with extensive coverage of nursing and healthcare research.
Search Strategies for Nursing Intervention Studies
Effective Keywords and MeSH Terms
- “nursing intervention”
- “patient outcomes”
- “evidence-based practice”
- “clinical effectiveness”
- “nursing care”
- “therapeutic intervention”
- “quality improvement“
Boolean Search Techniques
Use AND, OR, and NOT operators to refine searches:
- “nursing intervention” AND “patient outcomes”
- “evidence-based practice” OR “best practice”
- “nursing care” NOT “medical intervention”
Study Quality Assessment
Critical Appraisal Tools
- CASP (Critical Appraisal Skills Programme) – Provides checklists for different study types
- JBI Critical Appraisal Tools – Comprehensive assessment instruments
- GRADE (Grading of Recommendations Assessment) – Evaluates quality of evidence
Key Quality Indicators
- Sample size adequacy
- Randomization procedures
- Blinding methods
- Follow-up periods
- Statistical power
- Bias assessment
Major Categories of Nursing Interventions
1. Direct Patient Care Interventions
Studies examining medication error reduction, patient compliance, and therapeutic outcomes through improved nursing protocols.
Wound Care Management
Research on healing rates, infection prevention, and patient comfort through evidence-based wound care practices.
Pain Management
Investigations into pain assessment tools, non-pharmacological interventions, and patient-reported outcomes.
2. Patient Education and Support
Health Literacy Interventions
Studies measuring the impact of educational programs on patient understanding and self-care behaviors.
Discharge Planning
Research on readmission rates, patient satisfaction, and continuity of care through structured discharge interventions.
3. Technology-Enhanced Interventions
Telehealth Nursing
Studies examining remote patient monitoring, virtual consultations, and technology-mediated care delivery.
Electronic Health Records
Research on documentation efficiency, care coordination, and patient safety through EHR optimization.
Specific Examples of Effective Nursing Interventions
Emergency Department Interventions
Recent studies have shown that nursing interventions in the emergency department positively impact continuity of care, self-care, and psychological symptoms. These interventions include:
- Structured triage protocols
- Pain assessment standardization
- Family communication programs
- Discharge education protocols
Community Health Interventions
This is the first systematic review summarizing the evidence for the effectiveness of nurse-led interventions conducted by district nurses on community-living older people. Key interventions include:
- Home safety assessments
- Medication management programs
- Chronic disease monitoring
- Fall prevention protocols
Specialized Care Interventions
This review aimed to evaluate the effectiveness of nursing care interventions on various clinical outcomes in patients with pulmonary TB. Research demonstrates effectiveness in:
- Infection control measures
- Patient education programs
- Medication adherence support
- Symptom management protocols
Implementation Strategies for Evidence-Based Practice
Organizational Factors
Leadership Support
Strong administrative backing is crucial for successful implementation of evidence-based nursing interventions.
Resource Allocation
Adequate staffing, equipment, and training resources are essential for intervention success.
Culture of Innovation
Healthcare organizations must foster environments that encourage research utilization and continuous improvement.
Individual Factors
Knowledge and Skills
Nurses must possess the competencies necessary to locate, appraise, and apply research evidence.
Attitudes and Beliefs
Positive attitudes toward evidence-based practice significantly influence implementation success.
Confidence and Self-Efficacy
Nurses’ confidence in their ability to implement evidence-based interventions affects adoption rates.
Measuring Outcomes in Nursing Intervention Studies
Primary Outcome Measures
Clinical Outcomes
- Mortality rates
- Morbidity indicators
- Infection rates
- Readmission statistics
- Length of stay
Patient-Reported Outcomes
- Quality of life measures
- Patient satisfaction scores
- Functional status assessments
- Symptom severity ratings
Secondary Outcome Measures
Process Outcomes
- Adherence to protocols
- Documentation quality
- Communication effectiveness
- Care coordination measures
Economic Outcomes
- Cost per patient
- Resource utilization
- Staff productivity
- Return on investment
Challenges in Nursing Intervention Research
Methodological Challenges
Randomization Difficulties
Ethical and practical constraints often make randomization challenging in nursing research.
Blinding Issues
Many nursing interventions cannot be blinded, potentially introducing bias into study results.
Outcome Measurement
Standardized outcome measures for nursing interventions are often lacking or inadequate.
Implementation Challenges
Resource Constraints
Limited funding, staffing, and time can impede implementation of evidence-based interventions.
Resistance to change, hierarchical structures, and competing priorities can hinder adoption.
Knowledge Translation
Bridging the gap between research findings and clinical practice remains a significant challenge.
Future Directions in Nursing Intervention Research
Emerging Technologies
Artificial Intelligence
AI-powered tools are beginning to assist in intervention design, outcome prediction, and personalized care delivery.
Wearable Devices
Continuous monitoring technologies enable real-time assessment of intervention effectiveness.
Virtual Reality
VR applications are being studied for pain management, patient education, and therapeutic interventions.
Precision Nursing
Personalized Interventions
Research is moving toward individualized interventions based on patient characteristics and preferences.
Genomic Applications
Genetic factors are increasingly considered in intervention design and outcome prediction.
Predictive Analytics
Advanced analytics help identify patients most likely to benefit from specific interventions.
Practical Guidelines for Students and Researchers
Step-by-Step Approach to Study Analysis
- Define research question clearly
- Select appropriate databases
- Use systematic search strategies
- Document search process
2. Study Selection
- Apply inclusion/exclusion criteria
- Screen titles and abstracts
- Conduct full-text review
- Maintain detailed records
3. Quality Assessment
- Use standardized appraisal tools
- Evaluate study design appropriateness
- Assess risk of bias
- Consider clinical relevance
4. Data Extraction
- Create standardized forms
- Extract relevant information systematically
- Verify data accuracy
- Resolve discrepancies
5. Analysis and Synthesis
- Summarize key findings
- Identify patterns and themes
- Assess strength of evidence
- Draw appropriate conclusions
Common Pitfalls to Avoid
Selection Bias
Ensure comprehensive and systematic literature searches to avoid missing relevant studies.
Publication Bias
Consider unpublished studies and grey literature to obtain complete picture of evidence.
Confirmation Bias
Remain objective and consider findings that challenge preconceived notions.
Oversimplification
Recognize complexity of nursing interventions and avoid oversimplified interpretations.
Conclusion
Nursing intervention studies provide essential evidence for improving patient care and outcomes. By understanding how to locate, analyze, and apply findings from these studies, healthcare professionals can implement evidence-based practices that enhance patient safety, satisfaction, and clinical outcomes.
The field of nursing intervention research continues to evolve, with new methodologies, technologies, and approaches emerging regularly. Success in evidence-based practice requires ongoing commitment to learning, critical appraisal skills, and systematic approaches to research utilization.
For nursing students, researchers, and practicing professionals, mastering the skills necessary to work with nursing intervention studies is crucial for advancing the profession and improving patient care. Through systematic approaches to literature review, critical appraisal, and evidence synthesis, the nursing profession can continue to build its scientific foundation and enhance its impact on healthcare outcomes.
The evidence is clear: nursing interventions, when based on solid research evidence and implemented systematically, can significantly improve patient outcomes, reduce healthcare costs, and enhance the quality of care delivery. As the healthcare landscape continues to evolve, nursing intervention research will remain a cornerstone of professional practice and patient care excellence.
References
- Alshahrani, A., Alotaibi, A., Alsharari, A., & Alshahrani, F. (2024). The impact of evidence-based practice on patient outcomes: A systematic review. Journal of Evaluation in Clinical Practice, 30(2), 245-258. https://doi.org/10.1111/jep.13890
- Baumbusch, J., Kirkham, S. R., Khan, K. B., McDonald, H., Semeniuk, P., Tan, E., & Anderson, J. M. (2008). Pursuing common agendas: A collaborative model for knowledge translation between research and practice in clinical settings. Research in Nursing & Health, 31(2), 130-140. https://doi.org/10.1002/nur.20242
- Bianchi, M., Bagnasco, A., Bressan, V., Barisone, M., Timmins, F., Rossi, S., … & Sasso, L. (2018). A review of the role of nurse leadership in promoting and sustaining evidence-based practice. Journal of Nursing Management, 26(8), 918-932. https://doi.org/10.1111/jonm.12638
- Choi, M., Park, J. E., Lee, H. S., & Park, K. H. (2023). Effectiveness of nurse-led interventions on patient outcomes: A systematic review and meta-analysis. International Journal of Nursing Studies, 138, 104389. https://doi.org/10.1016/j.ijnurstu.2022.104389
- Dang, D., Dearholt, S. L., Bissett, K., Ascenzi, J., & Whalen, M. (2021). Johns Hopkins evidence-based practice for nurses and healthcare professionals: Model and guidelines (4th ed.). Sigma Theta Tau International. https://www.sigmamarketplace.org/johns-hopkins-evidence-based-practice-for-nurses-and-healthcare-professionals
- Fernandez, R., Johnson, M., Tran, D. T., & Miranda, C. (2012). Models of care in nursing: A systematic review. International Journal of Evidence-Based Healthcare, 10(4), 324-337. https://doi.org/10.1111/j.1744-1609.2012.00287.x
- Flodgren, G., O’Brien, M. A., Parmelli, E., & Grimshaw, J. M. (2019). Local opinion leaders: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, 6, CD000125. https://doi.org/10.1002/14651858.CD000125.pub4
- Grimshaw, J. M., Eccles, M. P., Lavis, J. N., Hill, S. J., & Squires, J. E. (2012). Knowledge translation of research findings. Implementation Science, 7(1), 50. https://doi.org/10.1186/1748-5908-7-50
- Harding, K. E., Porter, J., Horne-Thompson, A., Donley, E., & Taylor, N. F. (2014). Not enough time or a low priority? Barriers to evidence-based practice for allied health clinicians. Journal of Continuing Education in the Health Professions, 34(4), 224-231. https://doi.org/10.1002/chp.21255
- Harvey, G., & Kitson, A. (2016). PARIHS revisited: From heuristic to integrated framework for the successful implementation of knowledge into practice. Implementation Science, 11(1), 33. https://doi.org/10.1186/s13012-016-0398-2
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academy Press. https://www.nap.edu/catalog/10027/crossing-the-quality-chasm-a-new-health-system-for-the
- Kitson, A., Harvey, G., & McCormack, B. (1998). Enabling the implementation of evidence based practice: A conceptual framework. Quality in Health Care, 7(3), 149-158. https://doi.org/10.1136/qshc.7.3.149
- Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., … & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ, 339, b2700. https://doi.org/10.1136/bmj.b2700
- Melnyk, B. M., Gallagher‐Ford, L., Long, L. E., & Fineout‐Overholt, E. (2014). The establishment of evidence‐based practice competencies for practicing registered nurses and advanced practice nurses in real‐world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews on Evidence‐Based Nursing, 11(1), 5-15. https://doi.org/10.1111/wvn.12021
- Melnyk, B. M., & Fineout-Overholt, E. (2019). Evidence-based practice in nursing & healthcare: A guide to best practice (4th ed.). Wolters Kluwer. https://www.wolterskluwer.com/en/solutions/ovid/evidence-based-practice-in-nursing-healthcare-a-guide-to-best-practice
- National Institute for Health and Care Excellence. (2014). Developing NICE guidelines: The manual. NICE. https://www.nice.org.uk/process/pmg20/chapter/introduction
- Newhouse, R. P., Dearholt, S. L., Poe, S. S., Pugh, L. C., & White, K. M. (2017). Johns Hopkins nursing evidence-based practice: Model and guidelines (3rd ed.). Sigma Theta Tau International. https://www.sigmamarketplace.org/johns-hopkins-nursing-evidence-based-practice-model-and-guidelines
- Polit, D. F., & Beck, C. T. (2021). Nursing research: Generating and assessing evidence for nursing practice (11th ed.). Wolters Kluwer. https://www.wolterskluwer.com/en/solutions/ovid/nursing-research-generating-and-assessing-evidence-for-nursing-practice
- Rycroft-Malone, J., Seers, K., Titchen, A., Harvey, G., Kitson, A., & McCormack, B. (2004). What counts as evidence in evidence-based practice? Journal of Advanced Nursing, 47(1), 81-90. https://doi.org/10.1111/j.1365-2648.2004.03068.x
- Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. BMJ, 312(7023), 71-72. https://doi.org/10.1136/bmj.312.7023.71
- Squires, J. E., Sullivan, K., Eccles, M. P., Worswick, J., & Grimshaw, J. M. (2014). Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implementation Science, 9(1), 152. https://doi.org/10.1186/s13012-014-0152-6
- Stetler, C. B. (2001). Updating the Stetler model of research utilization to facilitate evidence-based practice. Nursing Outlook, 49(6), 272-279. https://doi.org/10.1067/mno.2001.120517
- Straus, S. E., Glasziou, P., Richardson, W. S., & Haynes, R. B. (2018). Evidence-based medicine: How to practice and teach EBM (5th ed.). Elsevier. https://www.elsevier.com/books/evidence-based-medicine/straus/978-0-7020-6296-4
- Titler, M. G. (2008). The evidence for evidence-based practice implementation. Patient Safety and Quality: An Evidence-Based Handbook for Nurses, 1, 1-49. https://www.ncbi.nlm.nih.gov/books/NBK2659/
- Wensing, M., Bosch, M., & Grol, R. (2010). Developing and selecting interventions for translating knowledge to action. Canadian Medical Association Journal, 182(2), E85-E88. https://doi.org/10.1503/cmaj.081233
Additional Database Sources
- CINAHL Complete (Cumulative Index to Nursing and Allied Health Literature) – https://www.ebsco.com/products/research-databases/cinahl-complete
- PubMed/MEDLINE – U.S. National Library of Medicine – https://pubmed.ncbi.nlm.nih.gov/
- Cochrane Library – Cochrane Collaboration – https://www.cochranelibrary.com/
- Scopus – Elsevier – https://www.scopus.com/
- Web of Science – Clarivate Analytics – https://www.webofscience.com/
- JBI Database of Systematic Reviews and Implementation Reports – https://journals.lww.com/jbisrir/
- Nursing Reference Center Plus – EBSCO – https://www.ebsco.com/products/research-databases/nursing-reference-center-plus
- ProQuest Nursing & Allied Health Database – https://www.proquest.com/products-services/nursing-allied-health-database.html
Professional Organizations and Guidelines
- American Nurses Association (ANA) – Evidence-Based Practice Guidelines – https://www.nursingworld.org/practice-policy/evidence-based-practice/
- International Council of Nurses (ICN) – Best Practice Guidelines – https://www.icn.ch/what-we-do/projects/evidenced-based-practice-guidelines
- Sigma Theta Tau International – Evidence-Based Practice Resources – https://www.sigmanursing.org/advance-elevate/ebp
- Academy Health – Implementation Science Guidelines – https://www.academyhealth.org/about/areas-of-expertise/implementation-science
- Joanna Briggs Institute – Systematic Review Methodology – https://jbi.global/
- National Institute for Health and Care Excellence (NICE) – Clinical Guidelines – https://www.nice.org.uk/guidance
Web Sources Referenced in Article
- Impact of an emergency department nursing intervention – https://pmc.ncbi.nlm.nih.gov/articles/PMC10768496/
- A Study on the Effect of Nursing Intervention Based – https://pmc.ncbi.nlm.nih.gov/articles/PMC9300328/
- Evidence-based interventions and nurse-sensitive – https://www.sciencedirect.com/science/article/pii/S2666142X21000357
- The Influence of Nursing Interventions on Patient Outcomes – https://karger.com/sjh/article/4/1/1/868530/The-Influence-of-Nursing-Interventions-on-Patient
- Nursing Intervention – an overview | ScienceDirect Topics – https://www.sciencedirect.com/topics/nursing-and-health-professions/nursing-intervention

