Table of Contents
ToggleEpidemiologic Triangle – Sample Expert Answer
The epidemiologic triangle is a fundamental model used in epidemiology to understand and explain the dynamics of disease transmission. It consists of three components: the agent, the host, and the environment. The agent is the microorganism or pathogen that causes the disease, such as bacteria, viruses, or parasites (Liu et al., 2023). The host refers to the individual who can become infected, whose susceptibility to disease can be influenced by factors such as age, immunity, and overall health. The environment encompasses the external factors that allow the disease to spread, such as climate, living conditions, and healthcare access.
To break the chain of transmission within the epidemiologic triangle, community health nurses can implement various nursing interventions. One effective intervention is vaccination campaigns. By increasing the immunity of the host population through vaccination, nurses reduce the number of susceptible individuals, thus limiting the spread of communicable diseases like influenza or measles (Xu et al., 2023). This breaks the link between the agent and the host, as fewer people are vulnerable to infection. Vaccination is a preventive measure that not only protects individuals but also contributes to herd immunity, reducing the overall disease burden in the community.
Another key nursing intervention is health education on safe food and water practices. For diseases transmitted through contaminated food or water, such as cholera or hepatitis A, educating the community about proper food handling, cooking, and safe water usage can break the link between the agent and the environment (Xu et al., 2023). Educating the public on these practices helps control the spread of disease and empowers individuals to take proactive steps to protect their health. These interventions are critical in preventing outbreaks, especially in underserved communities where access to clean water and sanitation may be limited.
References
Liu, J., Liu, M., & Liang, W. (2023). The ‘Triangle Model’theory for prevention and control of newly emerging infectious diseases: Definition, characteristics, and experience in China. Global Transitions, 5, 137-140. https://doi.org/10.1016/j.glt.2023.08.004
Xu, J., Abudurusuli, G., Rui, J., Li, Z., Zhao, Z., Xia, Y., … & Chen, T. (2023). Epidemiological characteristics and transmissibility of HPV infection: A long-term retrospective study in Hokkien Golden Triangle, China, 2013–2021. Epidemics, 44, 100707. https://doi.org/10.1016/j.epidem.2023.100707
Global Communicable Disease – Sample Expert Answer
One significant global communicable disease outbreak that has impacted community health worldwide is the COVID-19 pandemic. Emerging in late 2019, the virus rapidly spread across the globe, leading to widespread illness, significant mortality, and overwhelming healthcare systems (Advani et al., 2023). The affected population has been vast, encompassing all age groups, though older adults and individuals with pre-existing health conditions have been disproportionately impacted. The virus has caused severe respiratory illness, increased hospitalization rates, and economic hardship due to lockdowns and disruptions in daily life.
The progression of COVID-19 has been significantly influenced by social determinants of health (SDOH). Factors such as poverty, access to healthcare, education, and living conditions have played a critical role in the spread and severity of the disease. Individuals living in densely populated areas with limited access to healthcare or inadequate housing are more vulnerable to contracting the virus and experiencing worse outcomes (Salve et al., 2023).
In many regions, frontline workers and marginalized communities have experienced higher rates of infection and mortality due to their exposure and limited capacity to adopt preventive measures like social distancing or working from home.
A community health nurse working with populations impacted by COVID-19 can integrate a Christian worldview by emphasizing values of compassion, service, and holistic care. This can be exemplified through the nurse’s efforts to address both the physical and emotional needs of affected individuals, while providing spiritual support and encouragement (Salve et al., 2023). The nurse may advocate for equitable vaccine distribution in underserved communities, ensuring that vulnerable populations are not left behind.
Additionally, the Christian principle of loving one’s neighbor can guide the nurse in fostering community resilience by promoting health education, supporting mental health initiatives, and offering hope to individuals facing anxiety, grief, or isolation due to the pandemic.
References
Advani, S. D., Sickbert-Bennett, E., Moehring, R., Cromer, A., Lokhnygina, Y., Dodds-Ashley, E., … & CDC Prevention Epicenters Program. (2023). The disproportionate impact of coronavirus disease 2019 (COVID-19) pandemic on healthcare-associated infections in community hospitals: need for expanding the infectious disease workforce. Clinical Infectious Diseases, 76(3), e34-e41. https://doi.org/10.1093/cid/ciac684
Salve, S., Raven, J., Das, P., Srinivasan, S., Khaled, A., Hayee, M., … & Gooding, K. (2023). Community health workers and Covid-19: Cross-country evidence on their roles, experiences, challenges and adaptive strategies. PLOS Global Public Health, 3(1), e0001447. https://doi.org/10.1371/journal.pgph.0001447
 Limited Offer: Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Limited Offer: Use Coupon Code: NEW30 to Get 30% OFF Your First Order

Epidemiologic Triangle: Definition, Application, and Evidence-Based Nursing Interventions for Community Health Practice
Introduction
Community health nurses face complex challenges in disease prevention and health promotion. Understanding how diseases spread and implementing effective interventions requires a solid foundation in epidemiological principles. The epidemiologic triangle, also known as the epidemiological triad, serves as a cornerstone model for analyzing disease causation and developing targeted prevention strategies.
This comprehensive guide explores how to define the epidemiologic triangle, discuss its application to practice, and develop evidence-based nursing interventions that community health nurses can implement to break the links within this fundamental public health model. Whether you’re a nursing student seeking to understand these concepts or a practicing community health nurse looking to enhance your intervention strategies, this resource provides the theoretical knowledge and practical tools needed for effective disease prevention and health promotion.
What is the Epidemiologic Triangle? A Complete Definition
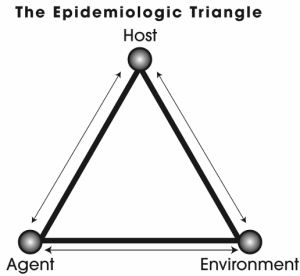
The epidemiologic triangle definition encompasses three interconnected components that work together to explain how diseases occur and spread within populations. This agent-host-environment model provides a systematic framework for understanding disease transmission and developing targeted interventions.
The Three Components of the Epidemiologic Triangle
1. Agent: The Causative Factor
The agent represents the causative factor that initiates disease or health conditions. Agents can be classified into several categories:
Biological Agents:
- Bacteria (e.g., Streptococcus, Salmonella)
- Viruses (e.g., influenza, COVID-19)
- Parasites (e.g., malaria, intestinal worms)
- Fungi (e.g., Candida, dermatophytes)
Physical Agents:
- Radiation exposure
- Extreme temperatures
- Mechanical forces causing injury
- Noise pollution
Chemical Agents:
- Toxins and poisons
- Environmental pollutants
- Occupational chemicals
- Pharmaceutical substances
Nutritional Agents:
- Vitamin deficiencies
- Mineral imbalances
- Malnutrition
- Excessive caloric intake
2. Host: The Susceptible Individual
The host refers to the person or population susceptible to the disease. Host factors influence an individual’s vulnerability to illness and include:
Intrinsic Factors:
- Age and developmental stage
- Genetic predisposition
- Immune system status
- Hormonal factors
- Nutritional status
Behavioral Factors:
- Lifestyle choices
- Health practices
- Risk-taking behaviors
- Compliance with preventive measures
Social Factors:
- Socioeconomic status
- Education level
- Cultural beliefs
- Access to healthcare
3. Environment: The Context for Disease Transmission
The environment encompasses all external factors that influence disease transmission and includes:
Physical Environment:
- Climate and weather conditions
- Geographic location
- Housing conditions
- Water and air quality
- Vector breeding sites
Social Environment:
- Population density
- Social networks
- Cultural practices
- Economic conditions
- Healthcare infrastructure
Temporal Environment:
- Seasonal patterns
- Time of day
- Duration of exposure
- Timing of interventions
Application of the Epidemiologic Triangle to Community Health Practice
Understanding Disease Causation and Transmission
The epidemiologic triangle application in practice involves analyzing how these three components interact to produce disease. Community health nurses use this model to:
- Identify Risk Factors: Assess which agents pose threats to specific populations
- Evaluate Host Susceptibility: Determine which individuals or groups are most vulnerable
- Analyze Environmental Conditions: Examine factors that facilitate or prevent disease transmission
- Develop Targeted Interventions: Create strategies that address one or more components of the triangle
Real-World Case Study: Tuberculosis Prevention
Consider a community health nurse working in an urban area with high tuberculosis (TB) rates:
Agent Analysis:
- Mycobacterium tuberculosis (bacterial agent)
- Airborne transmission through respiratory droplets
- Increased virulence in drug-resistant strains
Host Analysis:
- Vulnerable populations: immunocompromised individuals, elderly, malnourished
- Risk factors: HIV infection, diabetes, substance abuse
- Social determinants: poverty, homelessness, overcrowding
Environmental Analysis:
- Poor ventilation in housing
- Overcrowded living conditions
- Limited access to healthcare
- Seasonal patterns of transmission
Case Study: Childhood Obesity Prevention
A community health nurse addressing childhood obesity would analyze:
Agent Analysis:
- Excessive caloric intake (nutritional agent)
- Sedentary lifestyle patterns
- Processed food consumption
Host Analysis:
- Genetic predisposition to obesity
- Age-related metabolic changes
- Family history of diabetes
Environmental Analysis:
- Food deserts lacking healthy options
- Limited safe recreational spaces
- School nutrition programs
- Socioeconomic barriers to healthy eating
Evidence-Based Nursing Interventions to Break Epidemiologic Triangle Links
Community health nurses can implement multiple nursing interventions to disrupt disease transmission by targeting each component of the epidemiologic triangle. These interventions go beyond basic hygiene practices like handwashing to address complex health challenges.
Agent-Focused Interventions
1. Vaccination and Immunization Programs
Intervention Strategy: Develop and implement comprehensive vaccination campaigns targeting specific diseases within the community.
Implementation Steps:
- Conduct community needs assessments to identify vaccination gaps
- Collaborate with local healthcare providers and schools
- Organize mobile vaccination clinics for underserved populations
- Provide education about vaccine safety and efficacy
- Maintain accurate immunization records and follow-up systems
Evidence Base: Research demonstrates that community-wide vaccination programs can achieve herd immunity thresholds, significantly reducing disease transmission. The WHO estimates that immunization prevents 2-3 million deaths annually.
Breaking the Triangle: This intervention directly targets the agent by preventing pathogen establishment in the host population, effectively breaking the agent-host link.
2. Environmental Disinfection and Vector Control
Intervention Strategy: Implement systematic environmental controls to reduce pathogen survival and vector breeding.
Implementation Steps:
- Educate communities about proper disinfection techniques
- Coordinate with environmental health departments
- Implement integrated pest management programs
- Advocate for improved sanitation infrastructure
- Monitor and evaluate environmental interventions
Evidence Base: Studies show that environmental interventions can reduce disease transmission by up to 70% in some infectious disease outbreaks.
Breaking the Triangle: These interventions target both the agent (reducing pathogen survival) and the environment (eliminating transmission pathways).
Host-Focused Interventions
3. Health Education and Behavior Modification Programs
Intervention Strategy: Develop comprehensive health education programs that address specific risk behaviors and promote protective health practices.
Implementation Steps:
- Assess community health literacy levels
- Design culturally appropriate educational materials
- Implement peer education programs
- Use multiple communication channels (digital, print, community events)
- Evaluate behavior change outcomes
Evidence Base: Systematic reviews indicate that well-designed health education programs can improve health behaviors by 15-40% and reduce disease incidence by 10-25%.
Breaking the Triangle: This intervention strengthens the host’s resistance to disease by improving knowledge, attitudes, and protective behaviors.
4. Nutritional Counseling and Supplementation Programs
Intervention Strategy: Provide targeted nutritional interventions to improve host immunity and reduce disease susceptibility.
Implementation Steps:
- Conduct nutritional assessments in high-risk populations
- Develop individualized nutrition plans
- Coordinate with food assistance programs
- Provide nutrition education and cooking classes
- Monitor nutritional status and health outcomes
Evidence Base: Research shows that nutritional interventions can reduce infection rates by 20-30% in malnourished populations and improve overall health outcomes.
Breaking the Triangle: These interventions strengthen host resistance by improving nutritional status and immune function.
Environment-Focused Interventions
5. Community Environmental Health Advocacy
Intervention Strategy: Advocate for policy changes and environmental improvements that reduce disease transmission risks.
Implementation Steps:
- Identify environmental health hazards through community assessments
- Collaborate with local government and environmental agencies
- Organize community action groups
- Advocate for policy changes and resource allocation
- Monitor environmental improvements and health outcomes
Evidence Base: Environmental health interventions have been shown to reduce disease incidence by 25-50% in affected communities, particularly for waterborne and vector-borne diseases.
Breaking the Triangle: This intervention modifies the environment to reduce disease transmission opportunities and improve overall population health.
6. Social Determinants of Health Interventions
Intervention Strategy: Address underlying social and economic factors that influence health outcomes and disease susceptibility.
Implementation Steps:
- Conduct comprehensive community health assessments
- Identify social determinants affecting health outcomes
- Collaborate with social services and community organizations
- Advocate for policy changes addressing health inequities
- Develop programs addressing housing, employment, and education
Evidence Base: Interventions targeting social determinants can reduce health disparities by 30-50% and improve overall population health outcomes.
Breaking the Triangle: These interventions modify environmental factors (social environment) that influence both host susceptibility and disease transmission patterns.
Specific Nursing Interventions for Breaking Triangle Links
Breaking the Agent-Host Link
Intervention 1: Community-Based Screening and Early Detection Programs
Objective: Identify and treat disease agents before they can establish infection or progress to serious illness.
Implementation:
- Establish regular screening programs for high-risk populations
- Use point-of-care testing for rapid diagnosis
- Implement contact tracing for infectious diseases
- Provide immediate treatment or referral services
- Maintain confidential health records and follow-up systems
Measurable Outcomes:
- Percentage of population screened annually
- Number of cases detected early
- Reduction in disease complications
- Improvement in treatment success rates
Intervention 2: Targeted Prophylactic Treatment Programs
Objective: Prevent disease development in high-risk individuals through preventive treatment.
Implementation:
- Identify individuals at high risk for specific diseases
- Provide prophylactic medications or treatments
- Monitor for adverse effects and treatment compliance
- Educate about the importance of completing treatment
- Coordinate with healthcare providers for ongoing care
Measurable Outcomes:
- Reduction in disease incidence among treated populations
- Compliance rates with prophylactic treatments
- Adverse event rates
- Cost-effectiveness of intervention
Breaking the Host-Environment Link
Intervention 3: Community Resilience Building Programs
Objective: Strengthen community capacity to respond to health threats and maintain health-promoting environments.
Implementation:
- Develop community emergency preparedness plans
- Train community health workers and volunteers
- Establish community health coalitions
- Create sustainable funding mechanisms
- Implement community-led health initiatives
Measurable Outcomes:
- Community preparedness assessment scores
- Number of trained community health workers
- Participation rates in health programs
- Community health indicator improvements
Intervention 4: Environmental Health Monitoring and Improvement
Objective: Continuously monitor and improve environmental conditions that affect health outcomes.
Implementation:
- Establish environmental health surveillance systems
- Conduct regular environmental health assessments
- Advocate for environmental improvements
- Educate communities about environmental health risks
- Coordinate with environmental agencies and organizations
Measurable Outcomes:
- Environmental health indicator improvements
- Reduction in environmentally-related illnesses
- Community awareness levels
- Policy changes implemented
Implementation Strategies for Community Health Nurses
Assessment and Planning
Before implementing interventions, community health nurses must conduct comprehensive assessments:
- Community Health Assessment:
- Demographic analysis
- Health status indicators
- Environmental factors
- Social determinants of health
- Available resources and partnerships
- Epidemiologic Triangle Analysis:
- Identify relevant agents
- Assess host factors
- Evaluate environmental conditions
- Determine interaction patterns
- Priority Setting:
- Use data to identify highest-risk populations
- Consider resource availability
- Evaluate intervention feasibility
- Align with community priorities
Collaboration and Partnership Development
Successful interventions require strong partnerships:
- Healthcare Partners: Hospitals, clinics, primary care providers
- Government Agencies: Health departments, environmental agencies
- Community Organizations: Schools, faith-based organizations, social services
- Educational Institutions: Universities, nursing schools
- Private Sector: Businesses, foundations, healthcare corporations
Evaluation and Quality Improvement
Continuous evaluation ensures intervention effectiveness:
- Process Evaluation:
- Implementation fidelity
- Reach and participation rates
- Resource utilization
- Stakeholder satisfaction
- Outcome Evaluation:
- Health outcome improvements
- Behavioral changes
- Environmental improvements
- Cost-effectiveness analysis
- Impact Evaluation:
- Long-term health outcomes
- Population-level changes
- Policy impacts
- Sustainability assessment
Advanced Applications and Emerging Trends
Technology Integration
Modern community health nursing increasingly incorporates technology:
- Digital Health Platforms: Mobile health apps, telemedicine
- Data Analytics: Predictive modeling, surveillance systems
- Geographic Information Systems: Disease mapping, resource allocation
- Social Media: Health communication, behavior change campaigns
One Health Approach
The epidemiologic triangle concept is expanding to include:
- Human-Animal-Environment Interface: Zoonotic disease prevention
- Climate Change Adaptation: Environmental health resilience
- Global Health Security: Pandemic preparedness and response
- Antimicrobial Resistance: Coordinated prevention strategies
Measuring Success: Key Performance Indicators
Health Outcome Indicators
- Disease incidence and prevalence rates
- Mortality and morbidity statistics
- Quality of life measurements
- Health equity assessments
Process Indicators
- Program reach and coverage
- Intervention fidelity
- Stakeholder engagement levels
- Resource utilization efficiency
Impact Indicators
- Policy changes implemented
- Environmental improvements achieved
- Community capacity enhancement
- Sustainable program elements
Future Directions and Recommendations
Emerging Challenges
Community health nurses must prepare for:
- Climate Change Health Impacts: Extreme weather events, vector-borne diseases
- Aging Populations: Chronic disease management, healthcare access
- Health Inequities: Social determinants, environmental justice
- Infectious Disease Threats: Pandemic preparedness, antimicrobial resistance
Professional Development
Continuous learning opportunities include:
- Epidemiology Training: Advanced statistical methods, surveillance systems
- Community Engagement: Cultural competency, community organizing
- Technology Skills: Digital health platforms, data analysis
- Policy Advocacy: Legislative processes, health policy development
Conclusion and Key Takeaways
The epidemiologic triangle provides a powerful framework for understanding disease causation and developing effective nursing interventions in community health practice. By systematically analyzing the agent, host, and environment components, community health nurses can design targeted interventions that break the links between these elements and prevent disease transmission.
The nursing interventions outlined in this guide—from vaccination programs and health education to environmental advocacy and social determinants interventions—offer evidence-based strategies for improving population health outcomes. Success depends on thorough assessment, strong partnerships, continuous evaluation, and adaptation to emerging health challenges.
As community health nursing continues to evolve, the epidemiologic triangle remains relevant while expanding to address complex health challenges including climate change, health equity, and emerging infectious diseases. By maintaining focus on this fundamental model while embracing innovation and collaboration, community health nurses can continue to make significant contributions to population health and disease prevention.
The key to successful implementation lies in understanding that these interventions work best when implemented as part of comprehensive, community-centered approaches that address multiple determinants of health simultaneously. Through careful planning, strong partnerships, and continuous evaluation, community health nurses can effectively break the epidemiologic triangle links and create healthier, more resilient communities.

I am a professional nursing assignment expert offering comprehensive academic support to university nursing students across various institutions. My services are designed to help learners manage their workload effectively while maintaining academic excellence. With years of experience in nursing research, case study writing, and evidence-based reporting, I ensure every paper is original, well-researched, and aligned with current academic standards.
My goal is to provide dependable academic assistance that enables students to focus on practical training and career growth.
Contact me today to receive expert guidance and timely, high-quality nursing assignment help tailored to your academic needs.