Write a 2000-2500 word essay addressing each of the following points/questions. Support your

Module 1: Assignment
Remember to submit your work following the file naming convention FirstInitial.LastName_M01.docx. For example, J.Smith_M01.docx. Remember that it is not necessary to manually type in the file extension; it will automatically append.
Start by reading and following these instructions:
- Quickly skim the questions or assignment below and the assignment rubric to help you focus.
- Read the required chapter(s) of the textbook and any additional recommended resources. Some answers may require you to do additional research on the Internet or in other reference sources. Choose your sources carefully.
- Consider the discussion and the any insights you gained from it.
- Create your Assignment submission and be sure to cite your sources, use APA style as required, check your spelling.
Assignment:
The History of Healthcare Finance. Write a 2000-2500 word essay addressing each of the following points/questions. Support your ideas with at least three (3) scholarly citations in your essay. Use strict APA guidelines to format the paper. The cover page and reference page do not count towards the minimum word amount and an abstract and table of contents are not necessary and if included are not part of the overall word count.
- Healthcare finance has change drastically since 1950. Please discuss the changes that have occurred and the effect on healthcare delivery with each change.
Expert Answer and Explanation
The History of Healthcare Finance
The US healthcare finance has experienced many changes over the past seventy years. Papanicolas et al. (2018) noted that rapid advances in medical technology and science, budget-busting increases in health care expenditures fueled by public and private insurance, and substantial gains in health outcomes attributable to medical care have marked the financial changes in the US healthcare system in the past seven decades.
As the country struggles to get out of a multiyear economic and financial crisis, the public and policymakers have increasingly in on healthcare expenditures that are rising sharply (Waxman, 2012). In other words, since 1950, US healthcare finance has changed drastically regarding payment sources and objects of expenditure. This purpose has discussed the changes that have occurred in US healthcare finance since 1950 and how they have impacted healthcare delivery.
In the 1950s, various changes in US healthcare affected healthcare finance. For instance, the Revenue Act of 1954 excluded employers’ contributions to workers’ health plans from taxable income (Permanyer & Scholl, 2019). This law impacted healthcare delivery by ensuring that employees received various health services. In 1956, the military program was enacted to provide health insurance to family members of officers of the Armed forces. The change improved the accessibility of care to family members of Armed forces officers.
The 1960s marked a huge milestone in US healthcare finance. In 1960, the Federal Employees Health Benefits Plan (FEHBP) was formed to provide health insurance for federal workers (Permanyer & Scholl, 2019). This law improved federal workers’ access to care by reducing the cost of care. In 1965, President Johnson passed the Medicare and Medicaid programs and signed them into law, with Truman on his side. The two programs marked a fundamental healthcare finance change in the American healthcare system.
Medicare Part A was designed to pay for home health care, limited skilled nursing, and hospital care. Optional Medicare Part B was to support paying for physician care. Medicaid was a separate program. It was designed to help states cover healthcare services for long-term care, the disabled, and people from poor classes (Waxman, 2012). Medicare was developed for people aged 65 years and above, people with End-Stage Renal Disease, and certain younger people with disabilities. The program pays for hospital and medical costs.
Medicare Part A helps pay for a limited time at a skilled nursing facility after a hospital stay. This part also pays for some hospice and home health care (Malekinejad et al., 2018). Part B helps eligible people pay for services from care providers such as doctors, home health care, outpatient care, preventive services, and durable medical equipment. The program may also cover the cost of hearing, health and wellness programs, and dental care. It also pays for prescribed drugs.
Medicaid was developed to provide health coverage to some people with limited resources and income. This program is run by states with the help of the federal government. The mandatory benefits the federal government requires states to provide include physician services, inpatient and outpatient hospital services, home health services, and laboratory and x-ray services, among others (Waxman, 2012). Optional benefits include case management, prescription drugs, occupational therapy, and physical therapy.
The Medicare and Medicaid programs impacted healthcare finance by ensuring that older people aged 65 years and above, people with disabilities, individuals with End-Stage Renal Disease, and those with limited resources and finance access care at an affordable cost. Medicaid covers over 70 million American citizens today, and in 2014, it reimbursed about 50% of all hospitals’ medical expenses. The Congressional Budget Office forecasts that Medicare and Medicaid programs will survive indefinitely due to sweeping spending reforms that have been made.
The Medicaid program was amended in 1967 to include additional services to the program. The amendment allowed the program to provide insurance coverage to Americans not receiving cash assistance. The amendment also added Early and Periodic Screening and Diagnostic Testing (EPSDT) to the program. In 1972, Supplemental Security Income (SSI) program was created. The program was created to provide monthly payments to children and adults with disabilities whose resources or income are below federal financial limits.
The program also provided financial assistance to older people aged 65 and above without disabilities who meet the financial qualifications. This program impacted healthcare finance by providing older people and individuals with disabilities who are below the poverty line with the ability to access healthcare services at an affordable cost.
The program pays for the care costs of people who meet eligibility criteria. Two years later, Hawaii Prepaid Health Care Act was passed. This act required employers in Hawaii to cover any worker working for them for more than 20 hours a week. The law was amended in 1989 when the State Health Insurance Program was added to cover people not eligible for employer-based insurance or Medicaid. This law changed healthcare finance in Hawaii by allowing people who do not qualify for employer-based insurance or Medicaid to receive care funded by the state government.
In 1977, the Health Care Financing Administration (HCFA) was developed within the Department of Health, Education, and Welfare (HEW). The program was created to manage the federal government’s largest healthcare financing programs, evaluate authority, and exercise regulations designed to assure the quality of healthcare services for many people in the US. The program administers Medicare programs that buy medical care for 39 million disabled and elderly individuals. It also provides a Medicaid program operating jointly under the state and federal authority to offer care services to 33 million low-income people.
The creation of HCF ensured that federal and state authorities assign funds for Medicaid and Medicare to one organization, ensuring that the money is distributed properly. The change made it easy to get Medicaid and Medicare complaints. In 1980, the HEW was named the Department of Health and Human Services (DHHS). The Department of Education was separated from the DHHS, and the funds allocated to the DHHS were meant for health only. During the same year, the federal government provided federal funding to states to improve care and adoption assistance. This move ensured state governments had enough funds to support state-sponsored healthcare programs.
In 1983, Diagnostic Related Groups (DRGs) were introduced by Medicare as a payment system for hospital payments. This initiative improved healthcare finance by making it easy for hospitals to determine payor reimbursement rates and better control hospital costs by categorizing patients with similar clinical diagnoses. Emergency Medical Treatment and Active Labor Act (EMTALA) was enacted in 1986. This law greatly impacted healthcare finance, especially in the emergency department. The law requires hospitals in partnership with Medicate to screen and provide emergency treatment to all who come into their emergency rooms, even if they cannot pay.
The same year, Consolidated Omnibus Budget Reconciliation Act (COBRA) was enacted. This law changed healthcare finance by allowing workers who have lost their jobs to continue enjoying their health insurance plan for 18 months. Therefore, workers who have lost their jobs must not worry about their health and finances for one and a half years. Another vital law was created in the 1980s. The law is the Medicare Catastrophic Coverage Act (MCCA). MCCA was enacted in 1988. The law expanded Medicare coverage to include a cap on beneficiaries’ out-of-pocket expenses and prescription drugs.
In 1996, the Health Insurance Portability and Accountability Act (HIPAA). The law protects US workers by permitting them to carry their health insurance policies from employment to employment (Edemekong et al., 2018). It also allows employees to lose coverage and adjust to changes such as adoptions, births, and marriages by applying to a select group of health insurance plans. The law also blocks insurers from discriminating against people applying for plans because of health problems. The Mental Health Parity Act was enacted in the same year. The law improved health coverage for patients with mental health problems.
Personal Responsibility and Work Opportunity Act was also enacted in the same year. This law allowed the state governments to provide health coverage to children and parents at present Aid to Families with Dependent Children (AFDC) levels and higher. The law prohibited Medicaid from providing cover to legal immigrants within the first five years in the US, except when they need emergency care.
The State Children’s Health Insurance Program (S-CHIP) act was enacted as part of the Balanced Budget Act (BBA) in 1997. The law provided block grants to states allowing them to provide health coverage to low-income children above Medicaid eligibility levels. The law also allowed states to cover the health services of disabled workers whose incomes are up to 250% of the poverty level.
The Breast and Cervical Cancer Treatment and Prevention Act of 2000 expanded the Medicaid program. It allowed it to provide coverage to uninsured women who are receiving treatment for cervical or breast cancer if they have been diagnosed following the Center for Disease Control (CDC) screening program, regardless of resources or income. In 2003, the Medicare Prescription Drug Improvement and Modernization Act was enacted.
Pakizegee and Stefanacci (2018) noted that the act is the most significant expansion of Medicare since it was enacted. This low included prescription drug benefits. It mandated Medicare to provide cover for prescription drugs. The State of Massachusetts passed legislation to offer healthcare coverage to nearly all its residents in 2006.
The law needed the residents of Massachusetts to attain health insurance coverage and called for shared responsibility among employers, individuals, and the government in financing the expanded health coverage program. The program cut the uninsured rate by half within two years of its implementation.
In the same year, the City of San Francisco created the Healthy San Francisco program, which provided universal care to city residents. Mental Health Parity Act was amended in 2008. It required insurance companies to treat mental health problems, including alcohol and substance abuse disorders equality and physical problems when health policies cover both.
The last grand change in healthcare finance is the Affordable Care Act (ACA). This act greatly changed healthcare finance in the US. This law was a modified version of the all-inclusive coverage US presidents in the 1900s imagined. The act aimed to provide health insurance to the majority of US citizens. The act needs most Americans to apply for health insurance coverage. Individuals who have not applied for cover will be penalized. However, few protected groups are exempted from the penalty.
Companies that employ more than 200 employers are bound to offer their workers’ health insurance coverage under the law (Zhao et al., 2020). The act created the American Health Benefits Exchange allowing Americans to review and compare health insurance plans to identify the best plan. The act also provides healthcare professionals the opportunity to take parting in improving the delivery of care.
According to Zhao et al. (2020), the healthcare industry can benefit from programs that deliver effective and efficient services to the growing patient population while decreasing care expenses. The ACA led to the creation of accountable care organizations (ACOs). This value-based care program requires healthcare professionals to pay for the quality of care provided instead of quantity (Zhao et al., 2020). ACOs coordinate care for patients who have a specific health insurance program.
Conclusion
The US healthcare system has experienced a lot of changes in terms of healthcare finance since 1950. The first change was the Revenue Act of 1954 was enacted to exclude employers’ contributions to workers’ health plans from taxable income. The second important change was the creation of the Medicare and Medicaid programs. The two programs marked a fundamental healthcare finance change in the American healthcare system. The two programs provide health insurance coverage to more than 70 million Americans.
The HIPAA is another major healthcare reform that impacted health finance. The law protects US workers by permitting them to carry their health insurance policies from employment to employment. The ACA is recent major healthcare reform that impacted healthcare finance in the US. The act aimed to provide health insurance to the majority of US citizens. The act needs most Americans to apply for health insurance coverage. Individuals who have not applied for cover will be penalized.
References
Edemekong, P. F., Annamaraju, P., & Haydel, M. J. (2018). Health insurance portability and accountability act.
Malekinejad, M., Horvath, H., Snyder, H., & Brindis, C. D. (2018). The discordance between evidence and health policy in the United States: The science of translational research and the critical role of diverse stakeholders. Health Research Policy and Systems, 16(1), 1-21.
Monica Hendrix, M. J. (2019). Getting Health Care Costs Under Control While Improving Quality of Care: The Maryland Way. Journal of Health Care Finance.
Pakizegee, M., & Stefanacci, R. G. (2018). Value-based clinical pathways in the world of reference-priced Medicare Part B drugs. J Clin Pathways, 4(10), 38-39.
Papanicolas, I., Woskie, L. R., & Jha, A. K. (2018). Health care spending in the United States and other high-income countries. Jama, 319(10), 1024-1039.
Permanyer, I., & Scholl, N. (2019). Global trends in lifespan inequality: 1950-2015. PloS one, 14(5), e0215742.
Waxman, T. (2012). Financial and Business Management for the Doctor of Nursing Practice. Springer Publishing Co.
Zhao, J., Mao, Z., Fedewa, S. A., Nogueira, L., Yabroff, K. R., Jemal, A., & Han, X. (2020). The Affordable Care Act and access to care across the cancer control continuum: A review at 10 years. CA: A Cancer Journal For Clinicians, 70(3), 165-181.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon: NEW30 to Get 30% OFF Your First Order
Use Coupon: NEW30 to Get 30% OFF Your First Order

What was the first healthcare reform in the United States?
In the ever-evolving landscape of healthcare in the United States, the journey towards comprehensive reform has been both tumultuous and transformative. Understanding the history of healthcare reform in the U.S. is essential to grasp the context in which our current healthcare system operates. In this article, we delve into the intricacies of the first healthcare reform in the United States, tracing its origins, significance, and impact on the nation’s healthcare landscape.
The Pioneering Steps: The First Healthcare Reform in the United States
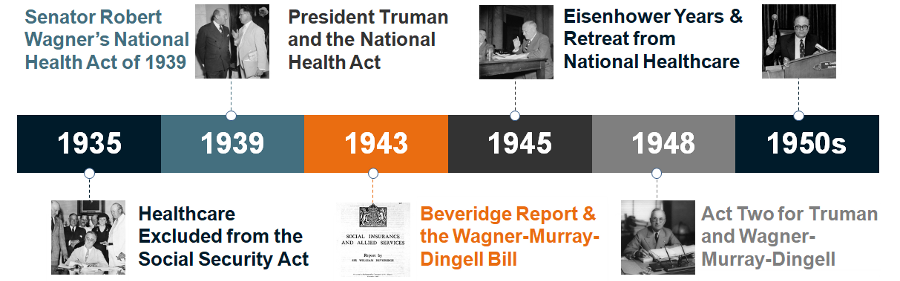
The journey towards healthcare reform in the United States had its roots in the early 20th century. The pivotal moment that marked the inception of comprehensive healthcare reform was the passage of the Social Security Act of 1935. Although not solely dedicated to healthcare, this landmark legislation laid the groundwork for the subsequent evolution of healthcare policies in the country.
The Social Security Act of 1935: A Game-Changer
The Social Security Act of 1935, signed into law by President Franklin D. Roosevelt, was a groundbreaking piece of legislation that aimed to provide a safety net for American citizens during times of economic hardship. While it primarily focused on establishing a system of old-age benefits and unemployment insurance, it also laid the foundation for healthcare reform through the creation of Social Security.
The Birth of Social Security
Under Title V of the Social Security Act, a program known as “Aid to Dependent Children” was introduced. This program marked the first federal foray into healthcare, as it provided financial assistance to states for maternal and child welfare services. This marked the earliest instance of the federal government’s involvement in healthcare.
The Significance of the Hill-Burton Act
While the Social Security Act of 1935 set the stage, the true catalyst for healthcare reform in the United States came in the form of the Hill-Burton Act, officially titled the Hospital Survey and Construction Act. This pivotal legislation was signed into law by President Harry S. Truman in 1946.
Expanding Access to Hospital Care
The Hill-Burton Act had a profound impact on healthcare infrastructure in the United States. It provided federal funding for the construction and modernization of hospitals, ensuring that communities across the nation had access to quality healthcare facilities. This was a crucial step in making healthcare services more accessible to the American populace.
Challenges and Progress: The Path Forward in Healthcare Reform
While the Social Security Act and the Hill-Burton Act laid the groundwork for healthcare reform, the journey towards a comprehensive healthcare system was far from over. In the subsequent decades, numerous challenges and significant milestones shaped the landscape of healthcare in the United States.
The Medicaid and Medicare Acts of 1965
One of the most significant advancements in healthcare reform came with the passage of the Medicaid and Medicare Acts in 1965. These acts, signed into law by President Lyndon B. Johnson, aimed to provide healthcare coverage to vulnerable populations, including the elderly and low-income individuals.
Medicaid: A Lifeline for the Vulnerable
Medicaid was established to provide healthcare coverage to low-income individuals and families. It represented a significant step towards achieving universal healthcare coverage, ensuring that those who couldn’t afford private insurance had access to essential medical services.
Medicare: Bridging Gaps in Healthcare for Seniors
Medicare, on the other hand, was designed to provide healthcare coverage to Americans aged 65 and older. This revolutionary program not only enhanced the quality of life for seniors but also played a crucial role in reducing the financial burden of healthcare costs in their later years.
The Affordable Care Act: A Landmark Achievement
In the 21st century, the United States witnessed another watershed moment in healthcare reform with the passage of the Patient Protection and Affordable Care Act, commonly known as the Affordable Care Act (ACA) or Obamacare, in 2010.
Expanding Healthcare Coverage
The ACA aimed to address several critical issues in the healthcare system, including expanding access to health insurance, improving the quality of care, and reducing healthcare costs. It introduced health insurance marketplaces, essential health benefits, and subsidies to make insurance more affordable for millions of Americans.
Conclusion: The Ongoing Journey
In conclusion, the first healthcare reform in the United States had its roots in the Social Security Act of 1935, which set the stage for federal involvement in healthcare. Subsequent legislation, such as the Hill-Burton Act, Medicaid, Medicare, and the Affordable Care Act, has contributed to the ongoing evolution of the nation’s healthcare system. These reforms have aimed to make healthcare more accessible, affordable, and equitable for all Americans.
As we navigate the complexities of healthcare reform, it’s essential to remember that the journey is far from over. The United States continues to grapple with the challenges of providing comprehensive healthcare coverage to its citizens. With each reform, we take another step towards achieving the goal of a healthier and more equitable nation.
History of Healthcare Reform in the United States
The history of healthcare reform in the United States is a complex and ongoing story that has evolved over centuries. This article will provide a concise overview of key milestones in the development of healthcare reform in the U.S., from its early beginnings to the present day.
Early Beginnings: The Colonial Period
The roots of healthcare reform in the United States can be traced back to the colonial period. In the 17th century, various colonies established laws to provide for the medical care of their residents. For example, the Massachusetts Bay Colony passed legislation in 1647 that required towns to appoint a local physician to care for the sick and injured. This early form of public healthcare laid the foundation for future reforms.
The Rise of Private Health Insurance
Throughout the 19th and early 20th centuries, healthcare in the United States was primarily a private matter. People paid for medical services out of pocket, and charitable organizations operated some hospitals. However, the need for a more comprehensive healthcare system became evident as the country’s population grew and industrialization brought new health challenges.
The Social Security Act of 1935
One of the most significant milestones in U.S. healthcare reform came with the passage of the Social Security Act of 1935 during the Great Depression. While primarily known for its establishment of Social Security benefits, this landmark legislation also provided federal funding for maternal and child health services. This marked the federal government’s first significant foray into healthcare.
Medicare and Medicaid: Expanding Access
In 1965, President Lyndon B. Johnson signed into law the Medicare and Medicaid programs as amendments to the Social Security Act. Medicare provided health insurance to Americans aged 65 and older, while Medicaid extended coverage to low-income individuals and families. These programs dramatically expanded access to healthcare services for vulnerable populations.
The Affordable Care Act (ACA)
The most recent major reform in U.S. healthcare occurred with the passage of the Patient Protection and Affordable Care Act, commonly known as the Affordable Care Act (ACA) or Obamacare, in 2010. This comprehensive legislation aimed to address several critical issues in the healthcare system, including:
- Expanding access to health insurance: The ACA created health insurance marketplaces where individuals and families could shop for coverage and receive subsidies to make insurance more affordable.
- Ensuring essential health benefits: The law required insurance plans to cover essential health benefits, such as preventive care, maternity care, and prescription drugs.
- Prohibiting discrimination: The ACA prohibited insurance companies from denying coverage or charging higher premiums based on pre-existing conditions.
- Expanding Medicaid: The ACA encouraged states to expand their Medicaid programs, providing coverage to more low-income individuals.
Challenges and Ongoing Debate
While these milestones represent significant progress in U.S. healthcare reform, challenges and debates persist. Access to healthcare remains a concern for many Americans, and the cost of medical care continues to be a contentious issue. Policymakers, healthcare professionals, and advocates continue to work towards improving the nation’s healthcare system to ensure that all citizens have access to quality and affordable care.
In conclusion, the history of healthcare reform in the United States is a story of evolution and adaptation to the changing needs of society. From early colonial efforts to the passage of landmark legislation like the Social Security Act, Medicare, Medicaid, and the ACA, the U.S. healthcare system has seen significant transformation. The ongoing debate about the future of healthcare reform reflects the importance of this issue in the lives of all Americans.
What is healthcare reform and why do we need it?
Healthcare Reform: Addressing the Need for Change
Healthcare reform refers to the process of making significant changes and improvements to the healthcare system of a country. It encompasses a wide range of policies, regulations, and initiatives aimed at enhancing the accessibility, affordability, and quality of healthcare services for all citizens. In the United States, healthcare reform has been a recurring topic of debate and action due to the recognition of various pressing issues within the healthcare system.
Why Do We Need Healthcare Reform?
- Access to Healthcare Services: One of the primary reasons for healthcare reform is to ensure that all individuals, regardless of their socioeconomic status, have access to necessary healthcare services. In the absence of reform, disparities in access can lead to preventable illnesses and even deaths among those who cannot afford or access medical care.
- Rising Healthcare Costs: Healthcare costs in the United States have been steadily increasing for decades. Without reform, these costs can become burdensome for individuals, families, and the overall economy. Reform aims to find ways to control and reduce healthcare expenses while maintaining or improving quality of care.
- Quality of Care: Healthcare reform efforts often focus on improving the quality of care provided by healthcare institutions and professionals. This includes implementing evidence-based practices, enhancing patient safety measures, and ensuring that healthcare providers adhere to high standards of care.
- Insurance Coverage: Reform seeks to expand insurance coverage to more people, reducing the number of uninsured or underinsured individuals. This is critical for ensuring that people have financial protection when they require medical services.
- Preventive Care: Many healthcare reform initiatives prioritize preventive care and wellness programs. By focusing on prevention, the healthcare system can reduce the incidence of costly and debilitating diseases, ultimately lowering healthcare expenditures.
- Eliminating Discrimination: Healthcare reform often includes provisions to eliminate discrimination in the healthcare system. This can involve ensuring that individuals with pre-existing conditions are not denied coverage and addressing disparities in care among different racial and ethnic groups.
- Streamlining Administrative Processes: Simplifying administrative processes within the healthcare system can lead to cost savings. Reform efforts may seek to reduce bureaucracy and administrative complexities.
- Innovation and Technology: Embracing innovation and technology is a key component of healthcare reform. Modernizing healthcare systems through electronic health records, telemedicine, and data analytics can improve efficiency and patient outcomes.
- Global Competitiveness: Many countries view a strong and efficient healthcare system as essential for economic competitiveness. Healthcare reform can help ensure that a nation’s workforce is healthy and productive.
- Social Equity: Healthcare reform aligns with the principle of social equity, where everyone has a fair opportunity to live a healthy life. It seeks to bridge gaps in healthcare access and outcomes, reducing disparities based on income, race, or geographic location.
In conclusion, healthcare reform is a multifaceted effort aimed at addressing various challenges within the healthcare system. It seeks to create a system that is more accessible, affordable, and equitable, while also promoting quality of care and the overall well-being of the population. Healthcare reform is an ongoing process that reflects the evolving needs and priorities of society.
What is the most recent health care reform passed in the US?
As of my last knowledge update in September 2021, the most recent major healthcare reform passed in the United States was the Patient Protection and Affordable Care Act (ACA), commonly known as Obamacare. It was signed into law by President Barack Obama on March 23, 2010. The ACA introduced significant changes to the U.S. healthcare system, with a focus on expanding access to healthcare, improving the quality of care, and controlling healthcare costs.
Key provisions of the Affordable Care Act included:
- Health Insurance Marketplaces: The ACA established state and federal health insurance marketplaces where individuals and families could compare and purchase private health insurance plans. These marketplaces also offered subsidies to help lower-income individuals and families afford coverage.
- Medicaid Expansion: The ACA encouraged states to expand their Medicaid programs to cover more low-income individuals and families. This expansion aimed to extend Medicaid eligibility to those who previously did not qualify for the program.
- Individual Mandate: The law included an individual mandate, which required most Americans to have health insurance coverage or pay a penalty on their federal taxes. This provision aimed to increase the number of people with insurance to help spread the risk and lower costs.
- Protections for Pre-existing Conditions: The ACA prohibited insurance companies from denying coverage or charging higher premiums based on pre-existing conditions. This provision aimed to ensure that individuals with health issues could still access insurance.
- Essential Health Benefits: Insurance plans offered through the marketplaces were required to cover essential health benefits, including preventive care, maternity care, prescription drugs, and more.
- Young Adult Coverage: The ACA allowed young adults to stay on their parents’ health insurance plans until the age of 26, providing coverage for many young people as they transitioned into adulthood.
It’s important to note that the healthcare landscape can change, and legislative developments may have occurred since my last knowledge update in September 2021. To get the most up-to-date information on healthcare reform in the United States, I recommend checking the latest news and government sources or consulting with a trusted healthcare policy expert or organization.
Why is health care reform so difficult in the US?
Healthcare reform in the United States is a complex and challenging endeavor for several interconnected reasons:
- Political Polarization: The U.S. has a highly polarized political landscape, and healthcare reform often becomes a partisan issue. Different political parties have divergent views on the role of government in healthcare, making it difficult to reach consensus on reform measures.
- Vested Interests: The healthcare industry in the U.S. is massive and includes insurance companies, pharmaceutical manufacturers, hospitals, and healthcare providers. These stakeholders have significant financial interests, which can influence policy decisions and make comprehensive reform difficult.
- Cost Concerns: Healthcare reform often involves discussions about how to control costs while expanding access and improving quality. Finding the right balance between cost containment and providing necessary care is a persistent challenge.
- Complexity of the System: The U.S. healthcare system is intricate, with multiple layers of government involvement, private insurance, and various programs. Simplifying and streamlining the system while maintaining its effectiveness is a daunting task.
- Federal vs. State Authority: Healthcare regulation is a shared responsibility between the federal government and individual states. This dual system can lead to disparities in access and coverage, as well as conflicting regulations.
- Resistance to Change: Any significant reform effort encounters resistance from those who fear changes in their current healthcare arrangements. This resistance can make it politically challenging to pass reform legislation.
- Public Opinion: Public opinion on healthcare reform can be divided. While many Americans express a desire for improved access and lower costs, there are differing views on how to achieve these goals. This diversity of perspectives can complicate the reform process.
- Legislative Process: The legislative process in the U.S. can be slow and cumbersome. Healthcare reform often involves complex bills that must pass through both houses of Congress and may face numerous amendments and debates.
- Historical Factors: The historical development of the U.S. healthcare system has created a patchwork of programs and regulations. Undoing or reforming aspects of this system requires navigating a complex web of precedents and interests.
- Budgetary Constraints: Healthcare reform initiatives often come with significant costs. Decisions about how to fund reform, whether through taxes, premiums, or other mechanisms, can be contentious and politically challenging.
- Legal Challenges: Major healthcare reform efforts, like the Affordable Care Act (ACA), have faced legal challenges that can further complicate their implementation and impact.
- Lobbying and Advocacy: Interest groups, including healthcare industry associations and advocacy organizations, play a significant role in shaping healthcare policy. Their influence on lawmakers can be substantial, making it challenging to enact reforms that face opposition from powerful interests.
Given these complexities and challenges, healthcare reform in the United States is a long and arduous process that requires a delicate balance between various stakeholders’ interests and political considerations. Successful reform efforts often involve compromise and incremental changes rather than sweeping, comprehensive overhauls of the entire system.


I am a professional nursing assignment expert offering comprehensive academic support to university nursing students across various institutions. My services are designed to help learners manage their workload effectively while maintaining academic excellence. With years of experience in nursing research, case study writing, and evidence-based reporting, I ensure every paper is original, well-researched, and aligned with current academic standards.
My goal is to provide dependable academic assistance that enables students to focus on practical training and career growth.
Contact me today to receive expert guidance and timely, high-quality nursing assignment help tailored to your academic needs.

