Last updated on July 1st, 2025 at 12:37 pm
Assignment Evidence-Based Project, Part 5: Recommending an Evidence-Based Practice Change
The collection of evidence is an activity that occurs with an endgame in mind. For example, law enforcement professionals collect evidence to support a decision to charge those accused of criminal activity. Similarly, evidence-based healthcare
In this Assignment, you will identify an issue or opportunity for change within your healthc
To Prepare:
- Reflect on the four peer-reviewed articles you critically appraised in Module 4, related to your clinical topic of interest and PICOT.
- Reflect on your current healthcare org
anization and think about potential opportunities for evidence-based change, using your topic of interest and PICOT as the basis for your reflection. - Consider the best method of disseminating the results of your presentation to an audience.
Create an 8- to 9-slide PowerPoint presentation in which you do the following:
- Briefly describe your healthcare organization, including its culture and readiness for change. (You may opt to keep various elements of this anonymous, such as your company name.)
- Describe the current problem or opportunity for change. Include in this description the circumstances surrounding the need for change, the scope of the issue, the stakeholders involved, and the risks associated with change implementation in general.
- Propose an evidence-based idea for a change in practice using an EBP approach to decision making. Note that you may find further research needs to be conducted if sufficient evidence is not discovered.
- Describe your plan for knowledge transfer of this change, including knowledge creation, dissemination, and organizational adoption and implementation.
- Describe the measurable outcomes you hope to achieve with the implementation of this evidence-based change.
- Be sure to provide APA citations of the supporting evidence-based peer-reviewed articles you selected to support your thinking.
- Add a lessons learned section that includes the following:
- A summary of the critical appraisal of the peer-reviewed articles you previously submitted
- An explanation about what you learned from completing the evaluation table (1 slide)
- An explanation about what you learned from completing the levels of evidence table (1 slide)
- An explanation about what you learned from completing the outcomes synthesis table (1 slide)
Expert Answer and Explanation
- I am currently working in a nursing and rehabilitation center, which mainly deals with patients with diverse needs. Our main task is to ensure that patients receive safe and quality care that will assist them regain independence and functionality like they were before their illness.
- The current organizational culture is unsupportive of the change with poor leadership, lack of accountability, and laxity by staff being some of the factors contributing to this culture.
- Currently the organization is having high number of cases of falls and other safety issues, which has drastically affected the facility’s rating, patient outcomes and to some extent even work satisfaction of the employees working within the facility. This problem can be attributed to lack of urgency shown by the staff when answering call-lights and alarms
- Scope: The issue mainly affects patients under admission, where at times they require help from the nurses but laxity of the nurses to respond to call lights and alarms, delay the help they require, which in most instances lead to adverse outcomes, like patient falls. The issue also mainly revolves around nursing unit, who are supposed to be at the forefront in responding to alarms and call lights.
- The change needed should therefore target at improving the response of nurses in tending to the sensory alarms and call lights to improve patient outcomes.
The stakeholders involved in the change include the following;
- The organization leadership – The organization leadership should show interest in the change given the impact of the issue on the performance of the organization. In support of the change, they should allocate the necessary resources needed to implement the change, and also be at the forefront in leading the change.
- Another stakeholder are the nurses, nurse practitioners and physicians who are in charge of delivering care to patients. They are supposed to actively participate in resolving the issue with the aim of improving patient outcomes.
- Technicians will also be among the stakeholders involved. Their role will be to ensure that the monitoring systems are properly functional to avoid false positives and false negatives which end up causing alarm fatigue and laxity by nurses to respond (Baker & Rodger, 2020).
- Quality assurance team should also be part of the initiative, with their role being to provide oversight on whether the change is meeting the intended quality- related outcomes
- The patients are also key stakeholders involved given that impact of the change in their outcomes.
- Some of the risks attached to implementing the proposed change include change resistance from nurses which will affect the success of the project. The other risk is increased nurse workload from what is currently is due to the requirement to increase their level of responses to sensory alarms and call lights. As it currently is, the nurses and other care providers have a lax attitude to respond to call lights and sensory alarms.
One of the main causes of laxity to respond to sensory alarms and call lights by nurses can be attributed to alarm fatigue (Baker & Rodger, 2020). Studies have indicated that sensory alarms fatigue is caused by faulty monitoring systems, inadequate training on how to respond to the sensory alarms and organizational factors including poor culture and leadership (Bach et al. , 2018).
Therefore the evidence based change that is suggested is to train nurses and introduce an online monitoring system that will reduce the number of false alarms, in turn improving response times and reducing alarm fatigue. The suggested intervention is linked with various studies as being effective including studies by Bach et al.
(2018) and Ruskin and Hueske-Kraus (2015).
To facilitate knowledge transfer for the change the following plan will be used. The first step is knowledge creation which will entail collection of evidence on good practices which can assist to improve nurse response times to sensory alarms. Knowledge will be created by collecting evidence on the current practice and its impact on patient outcomes and comparing it with best practices, through which the change initiative will be created.
The second step is to disseminate the knowledge to various stakeholders using various platforms including through meetings, print media and group discussion. The third stage is organizational adoption which will involve training on the best practices, that is the importance of prompt response to call lights and how to react on the new monitoring system that aims to eliminate alarm fatigue whose efficacy has been indicated by Bach et al.
(2018), before they are implemented.
The last stage is implementation, which will involve collective effort by the stakeholders led by the leadership, within the leadership to ensure successful implementation of a more responsive system to call lights and sensory alarms. Implementation will last for 3 months.
Some of the measurable outcomes that the evidence based change will aim to achieve include better response times by the nurses, reduction of fall incidents within the facility, improved rating of the facility and improved patient experience.
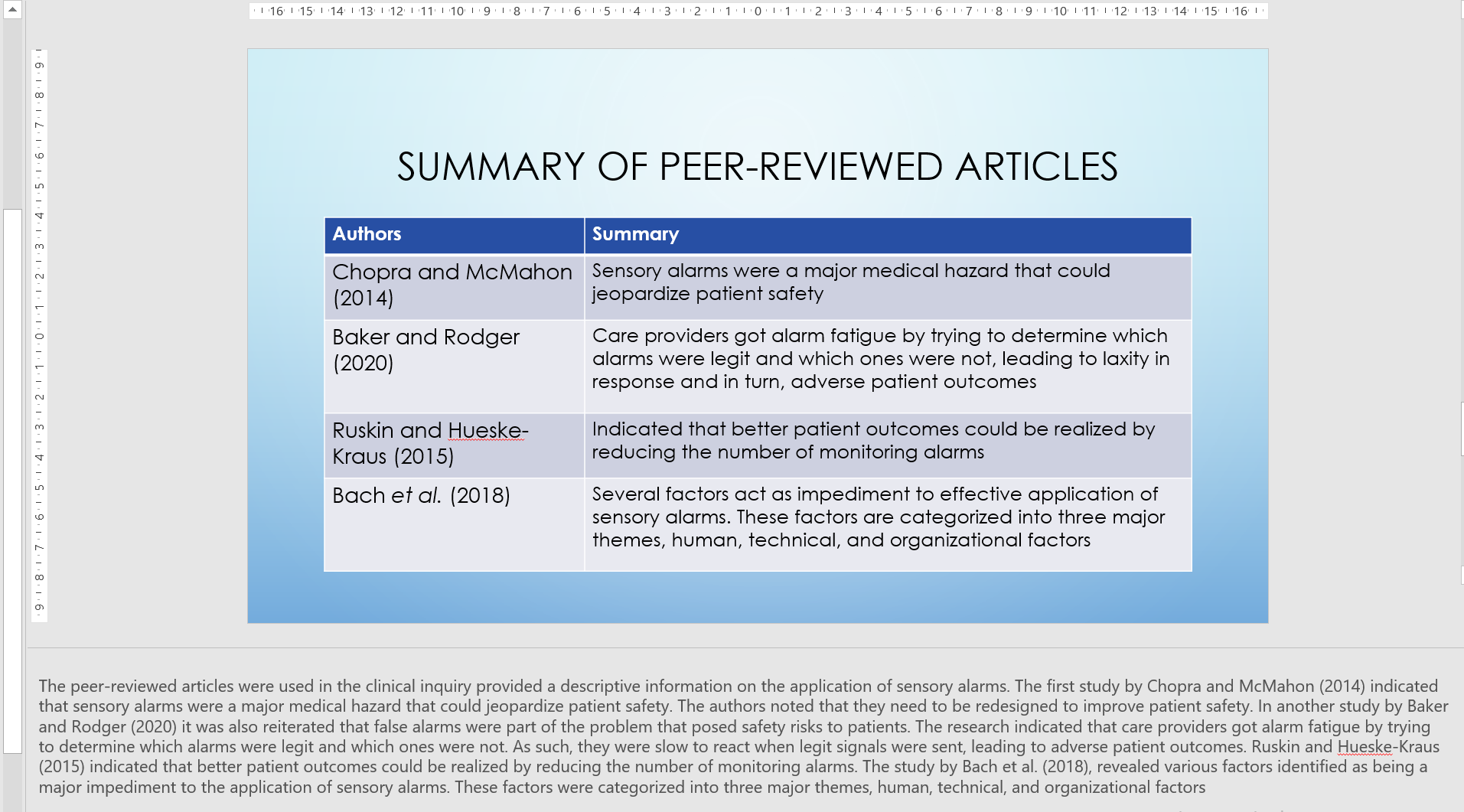
The peer-reviewed articles were used in the clinical inquiry provided a descriptive information on the application of sensory alarms. The first study by Chopra and McMahon (2014) indicated that sensory alarms were a major medical hazard that could jeopardize patient safety. The authors noted that they need to be redesigned to improve patient safety.
In another study by Baker and Rodger (2020) it was also reiterated that false alarms were part of the problem that posed safety risks to patients. The research indicated that care providers got alarm fatigue by trying to determine which alarms were legit and which ones were not. As such, they were slow to react when legit signals were sent, leading to adverse patient outcomes.
Ruskin and Hueske-Kraus (2015) indicated that better patient outcomes could be realized by reducing the number of monitoring alarms. The study by Bach et al. (2018), revealed various factors identified as being a major impediment to the application of sensory alarms.
Some of the lessons learned after completing the evaluation table include evaluation of evidence of in form best practices. Using the evaluation table, I was able to assess various forms of evidence and their relevance in informing a practice change.
Completion of the evaluation table also helped tome to learn different search strategies which improved my efficiency in collecting relevant evidence. The third lesson I learned was assessing articles based on their level of evidence.
References
- Bach, T. A., Berglund, L. M., & Turk, E. (2018). Managing alarm systems for quality and safety in the hospital setting. BMJ open quality, 7(3), e000202. https://doi.org/10.1136/bmjoq-2017-000202
- Baker, K., & Rodger, J. (2020). Assessing causes of alarm fatigue in long-term acute care and its impact on identifying clinical changes in patient conditions. Informatics in Medicine Unlocked, 18, 100300. https://doi.org/10.1016/j.imu.2020.100300
- Chopra, V., & McMahon, L. F. (2014). Redesigning hospital alarms for patient safety: alarmed and potentially dangerous. Jama, 311(12), 1199-1200. DOI: 10.1001/jama.2014.710
- Ruskin, K. J., & Hueske-Kraus, D. (2015). Alarm fatigue: impacts on patient safety. Current opinion in anaesthesiology, 28(6), 685–690. https://doi.org/10.1097/ACO.0000000000000260
Place your order now on a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers.

FAQs
14 Effective Ways to Implement Change in Healthcare
Implementing change in healthcare is a complex and multifaceted process that requires careful planning, collaboration, and consideration of various factors.
Identify the Need for Change: Define the specific problem or opportunity that requires change. This could be a clinical issue, operational inefficiency, patient safety concern, or a need to adapt to new regulations.
Form a Change Management Team: Assemble a multidisciplinary team that includes clinicians, administrators, IT experts, and other relevant stakeholders. This team will drive the change initiative and provide diverse perspectives.
Set Clear Objectives: Define clear and achievable goals for the change initiative. Make sure these objectives are measurable and aligned with the overall mission and values of the healthcare organization.
Develop a Comprehensive Plan: Create a detailed plan that outlines the steps, timeline, resources, and responsibilities for each phase of the change initiative. Consider potential risks and develop strategies to mitigate them.
Engage Stakeholders: Communicate the need for change to all relevant stakeholders, including staff, patients, families, and external partners. Address their concerns, provide opportunities for feedback, and involve them in the decision-making process.
Build a Supportive Culture: Foster a culture of openness, collaboration, and continuous improvement. Encourage staff to embrace change by providing training, resources, and a safe environment for experimentation.
Provide Training and Education: Ensure that staff members are equipped with the necessary skills and knowledge to adapt to the new processes or technologies. Offer training sessions, workshops, and resources to support their learning.
Pilot Testing: Before implementing change on a large scale, conduct pilot tests or small-scale trials to identify any potential issues or areas for improvement. Use feedback from these tests to refine your approach.
Monitor Progress and Adapt: Regularly track the progress of the change initiative against your established objectives. Be prepared to adjust your plan if you encounter unexpected challenges or if data suggests that modifications are needed.
Celebrate Successes: Recognize and celebrate milestones and achievements throughout the implementation process. This helps boost morale and reinforces the positive aspects of the change.
Address Resistance: Anticipate that some individuals might resist the change due to various reasons such as fear of the unknown or concerns about disruption. Address resistance empathetically, providing information, addressing concerns, and involving resisters in the decision-making process.
Communicate Continuously: Maintain transparent and ongoing communication throughout the implementation process. Keep stakeholders informed about progress, changes, and any adjustments to the plan.
Evaluate and Learn: After the change has been fully implemented, conduct a thorough evaluation to assess its impact on patient outcomes, operational efficiency, and other relevant metrics. Use this information to learn and improve for future change initiatives.
Iterate and Refine: Use the insights gained from the evaluation to refine your processes, address any remaining issues, and continuously improve the implemented change.
Successful Change Implementation in Healthcare
Change is inevitable in healthcare. New technologies, evolving patient populations, and shifting reimbursement models all demand that healthcare organizations constantly adapt and improve. However, change can be difficult to implement in healthcare, where there is often a culture of resistance to change and a lack of resources.
Despite the challenges, successful change implementation is possible in healthcare. Here are some key factors that contribute to successful change implementation in healthcare:
Clear and compelling vision for change. The first step to successful change implementation is to create a clear and compelling vision for the change. This vision should be communicated to all stakeholders and should articulate the benefits of the change for patients, providers, and the organization as a whole.
Engaged and committed leadership. Leadership support is essential for successful change implementation. Leaders must be visible champions of the change and must create a culture that supports change. They must also provide the resources and support needed to make the change successful.
Active participation of stakeholders. Stakeholders, such as staff, patients, and families, must be actively involved in the change process. This involvement will help to ensure that the change is relevant and that it meets the needs of all stakeholders.
Effective communication. Communication is key to successful change implementation. Leaders must communicate the vision for change clearly and consistently to all stakeholders. They must also be transparent about the challenges of change and must address concerns and resistance.
Flexibility and adaptability. The change process is often unpredictable and there will be challenges along the way. It is important to be flexible and adaptable in order to overcome these challenges.
Measurement and evaluation. It is important to measure and evaluate the progress of the change process on an ongoing basis. This will help to ensure that the change is on track and that it is having the desired impact.
By following these key factors, healthcare organizations can increase their chances of successful change implementation. Change can be difficult, but it is essential for healthcare organizations to adapt and improve in order to meet the needs of their patients.
In addition to the key factors listed above, there are a number of other strategies that can help to ensure successful change implementation in healthcare. These strategies include:
Using a change management framework. There are a number of change management frameworks that can be used to guide the change process. These frameworks can help to ensure that the change process is systematic and that all stakeholders are involved.
Creating a change champions network. A change champions network can be a valuable resource for successful change implementation. This network can be made up of staff, patients, families, and other stakeholders who are committed to the change. The change champions network can help to spread the word about the change, address concerns, and overcome resistance.
Using pilot projects. Pilot projects can be a great way to test out a change before it is implemented on a larger scale. This can help to identify and address any potential problems before they impact the entire organization.
Providing training and support. It is important to provide training and support to staff who are affected by the change. This training should help staff to understand the change, to develop new skills, and to overcome any challenges.
Celebrating successes. It is important to celebrate successes along the way. This will help to keep momentum going and to motivate staff to continue with the change process.
By following these strategies, healthcare organizations can increase their chances of successful change implementation. Change can be difficult, but it is essential for healthcare organizations to adapt and improve in order to meet the needs of their patients.
10 Examples of Organizational Change in Healthcare
The adoption of electronic health records (EHRs). EHRs are digital systems that store patient information, such as medical history, medications, and allergies. They have the potential to improve the quality and efficiency of care by making it easier for providers to access patient information and coordinate care. However, the adoption of EHRs has been a major challenge for healthcare organizations, as it requires a significant investment in time and money.
The rise of telehealth. Telehealth is the delivery of healthcare services through telecommunications technologies. It allows patients to receive care from providers remotely, through video conferencing or phone calls. Telehealth has become increasingly popular in recent years, as it can provide patients with convenient and affordable access to care.
The growth of integrated care delivery models. Integrated care delivery models bring together different types of healthcare providers, such as primary care physicians, specialists, and community health workers, to provide coordinated care to patients. This can help to improve the quality of care and reduce costs.
The increasing focus on patient engagement. Patient engagement is the active involvement of patients in their own care. It can be achieved through a variety of strategies, such as providing patients with educational materials, encouraging them to ask questions, and giving them a say in their treatment plans. Patient engagement can help to improve patient satisfaction, adherence to treatment, and health outcomes.
The use of predictive analytics and artificial intelligence (AI). Predictive analytics and AI are being used in healthcare to improve decision-making, identify patients at risk, and personalize care. For example, predictive analytics can be used to identify patients who are likely to experience complications after surgery, and AI can be used to develop chatbots that can provide patients with information and support.
The focus on population health. Population health is the health of a defined group of people, such as a community or a population. Healthcare organizations are increasingly focusing on population health, as it can help to improve the health of the entire community and reduce healthcare costs.
The emergence of value-based care. Value-based care is a reimbursement system that rewards healthcare organizations for providing high-quality, efficient care. It is designed to shift the focus from volume to value, and it is expected to have a major impact on the way healthcare is delivered.
The expansion of community health programs. Community health programs are designed to improve the health of the community by addressing social determinants of health, such as poverty, lack of education, and access to healthy food. These programs are becoming increasingly important, as they can help to reduce healthcare costs and improve population health.
The growth of accountable care organizations (ACOs). ACOs are groups of healthcare providers that work together to provide coordinated care to patients. They are responsible for the overall health of their patients, and they are rewarded for providing high-quality, efficient care.
The development of new payment models. New payment models are being developed that reward healthcare organizations for providing high-quality, efficient care. These models are designed to change the way healthcare is delivered and to improve the value of care.
10 Ways to Deal with Resistance to Change in Healthcare
The healthcare industry is constantly changing, and it can be difficult to get everyone on board with new initiatives. This is especially true when the change is perceived as a threat to the status quo.
Here are 10 ways to deal with resistance to change in healthcare:
Understand the reasons for resistance. The first step to overcoming resistance is to understand why people are resisting in the first place. Some common reasons for resistance to change in healthcare include:
- Fear of the unknown
- Uncertainty about the future
- Concerns about job security
- Lack of trust in the change leaders
- Past experiences with failed change initiatives
Communicate effectively. Communication is key to any successful change initiative. Make sure that you communicate the need for change clearly and concisely. Explain the benefits of the change, and address any concerns that employees may have.
Involve employees in the change process. When employees feel like they have a say in the change process, they are more likely to be supportive of it. Get input from employees early on, and make sure that they are involved in the decision-making process.
Provide training and support. Change can be difficult, and it’s important to provide employees with the training and support they need to succeed. This may include training on new procedures, software, or equipment. It’s also important to be patient and understanding, and to offer support to employees who are struggling with the change.
Celebrate successes. When employees see that the change is having a positive impact, they are more likely to continue supporting it. Make sure to celebrate successes along the way, and to recognize employees for their contributions.
Be patient. Change takes time. Don’t expect everyone to embrace the change overnight. Be patient and persistent, and continue to communicate and support employees throughout the process.
Be flexible. Things don’t always go according to plan. Be prepared to adjust the change plan as needed. If something isn’t working, don’t be afraid to make changes.
Get buy-in from leadership. Change is more likely to succeed if it has the support of senior leadership. Make sure that the change is communicated to and supported by all levels of leadership.
Use a change management process. There are a number of change management processes that can be used to help overcome resistance to change. Choose a process that is appropriate for the size and complexity of the change.
Don’t give up. Change is hard, but it’s important to remember that it’s necessary for growth and improvement. Don’t give up on the change, even if there is resistance. Keep communicating, supporting, and celebrating successes, and eventually you will overcome the resistance and achieve your goals.
10 Tips to Communicate a Change in Practice to Patients
Communicating a change in practice to patients can be a challenge. Patients may be hesitant to accept change, especially if it means they have to do something differently or if they feel like they are losing control of their care. However, it is important to communicate changes in practice in a clear, concise, and compassionate way in order to ensure that patients understand the reasons for the change and how it will affect them.
Here are 10 tips for communicating a change in practice to patients:
Start by explaining why the change is necessary. Patients are more likely to accept a change if they understand the reasons for it. Explain the rationale behind the change in a clear and concise way, using language that the patient can understand.
Address any concerns that the patient may have. Patients may have concerns about the change, such as how it will affect their care or their costs. Take the time to address these concerns in a thoughtful and empathetic way.
Be honest and transparent. Don’t sugarcoat the change or try to hide any potential downsides. Be honest with the patient about the pros and cons of the change, so that they can make an informed decision.
Use plain language. Avoid using medical jargon or technical terms that the patient may not understand. Use plain language that the patient can easily understand.
Be patient. It may take some time for the patient to adjust to the change. Be patient and understanding, and answer any questions that the patient may have.
Repeat the information. It is helpful to repeat the information about the change to the patient several times. This will help the patient to remember the information and to ask any questions that they may have.
Provide written materials. Providing the patient with written materials about the change can be helpful. This will give the patient something to refer to if they have any questions.
Follow up with the patient. After the change has been implemented, it is important to follow up with the patient to see how they are doing. This will give you the opportunity to answer any questions that they may have and to make sure that they are satisfied with the change.
Be prepared to answer questions. The patient may have a lot of questions about the change. Be prepared to answer these questions in a clear and concise way.
Be flexible. The patient may not be ready to accept the change right away. Be flexible and willing to work with the patient to make the change as smooth as possible.
By following these tips, you can communicate a change in practice to patients in a clear, concise, and compassionate way. This will help to ensure that patients understand the change and that they are satisfied with the outcome.