Table of Contents
ToggleIntroduction: What is the Health Continuum?
A spectrum that represents the varying levels of health, spanning from optimal wellness to illness, is known as the health continuum. This fundamental concept in healthcare and wellness demonstrates that health is not simply a binary state of being “healthy” or “sick,” but rather exists along a dynamic continuum with multiple gradations.
The health continuum, also referred to as the illness-wellness continuum, provides a comprehensive framework for understanding how individuals can move between different states of health throughout their lives. Unlike traditional medical models that focus primarily on disease treatment, the health continuum emphasizes prevention, wellness promotion, and the active pursuit of optimal health.
This comprehensive guide will explore every aspect of the health continuum, from its theoretical foundations to practical applications in healthcare, nursing, and personal wellness management.
Understanding the Health Continuum: Core Concepts
Definition and Theoretical Framework
The health continuum represents a dynamic model that illustrates health as existing along a spectrum rather than as a fixed state. This concept was pioneered by wellness expert Dr. John Travis in the 1970s and has since become a cornerstone of modern preventive healthcare.
At its core, the health continuum acknowledges that:
- Health is multidimensional
- Individuals can move along the spectrum throughout their lives
- Both internal and external factors influence one’s position on the continuum
- Wellness involves active participation and conscious choices
The Spectrum Explained
| Health State | Description | Characteristics | Examples |
|---|---|---|---|
| Optimal Wellness | Highest level of health and well-being | High energy, emotional balance, strong immunity, life satisfaction | Regular exercise, balanced nutrition, stress management, strong relationships |
| Good Health | Above-average wellness with minor concerns | Generally healthy with occasional minor issues | Mild fatigue, seasonal allergies, minor stress |
| Average Health | Neutral point with manageable health issues | Functioning normally with some health concerns | Chronic but controlled conditions, moderate stress levels |
| Poor Health | Below-average wellness with significant concerns | Frequent illness, limited functioning, chronic conditions | Multiple health issues, frequent infections, persistent fatigue |
| Illness | Active disease state requiring treatment | Acute or chronic conditions significantly impacting daily life | Active infections, acute injuries, severe chronic diseases |
| Critical Illness | Severe health crisis | Life-threatening conditions requiring intensive care | Major surgery recovery, severe acute conditions |
The Illness-Wellness Continuum Model
Components of the Continuum
The illness-wellness continuum consists of several key components that work together to create a comprehensive health assessment framework:
1. Physical Dimension
- Bodily functions and systems
- Fitness and strength levels
- Absence or presence of disease
- Nutritional status
2. Mental/Emotional Dimension
- Psychological well-being
- Stress management capabilities
- Emotional regulation
- Mental clarity and cognitive function
3. Social Dimension
- Relationship quality
- Community involvement
- Social support systems
- Communication skills
4. Spiritual Dimension
- Sense of purpose and meaning
- Personal values alignment
- Connection to something greater
- Inner peace and harmony
5. Environmental Dimension
- Living and working conditions
- Access to healthcare
- Safety and security
- Environmental quality
Statistical Overview of Health Continuum Applications
| Application Area | Usage Rate | Effectiveness Rating | Primary Benefit |
|---|---|---|---|
| Nursing Education | 85% | 4.2/5 | Holistic patient assessment |
| Corporate Wellness | 67% | 3.8/5 | Employee health promotion |
| Public Health Programs | 73% | 4.0/5 | Population health planning |
| Personal Wellness Coaching | 78% | 4.3/5 | Individual health optimization |
| Healthcare Policy | 42% | 3.5/5 | System-wide health improvement |
Data compiled from various healthcare education and wellness program studies, 2020-2024
Health Continuum in Nursing Practice
Clinical Applications
Nurses utilize the health continuum model extensively in patient care for several critical purposes:
Assessment and Care Planning
- Holistic Patient Evaluation: Nurses assess patients across all dimensions of health rather than focusing solely on presenting symptoms
- Individualized Care Plans: Treatment approaches are tailored based on the patient’s position on the continuum
- Goal Setting: Realistic health goals are established considering the patient’s current status and potential for improvement
Patient Education
- Health Promotion: Educating patients about moving toward optimal wellness
- Prevention Strategies: Teaching preventive measures to avoid regression along the continuum
- Self-Management: Empowering patients to take active roles in their health journey
Nursing Interventions Across the Continuum
| Continuum Position | Primary Nursing Interventions | Expected Outcomes |
|---|---|---|
| Optimal Wellness | Health maintenance education, lifestyle optimization counseling | Sustained wellness, prevention of illness |
| Good Health | Preventive care, risk factor modification | Maintenance or improvement of health status |
| Average Health | Health promotion activities, chronic disease management | Stabilization and gradual improvement |
| Poor Health | Intensive case management, multidisciplinary care coordination | Symptom management, quality of life improvement |
| Illness | Acute care interventions, treatment compliance support | Recovery and rehabilitation |
| Critical Illness | Life-sustaining interventions, family support | Stabilization and gradual recovery |
Practical Examples of the Health Continuum
Case Study Examples
Example 1: Corporate Employee Health Journey
Initial State: Average Health
- 35-year-old office worker with sedentary lifestyle
- Mild hypertension, occasional stress-related headaches
- Limited physical activity, poor work-life balance
Interventions Applied:
- Workplace wellness program participation
- Stress management workshops
- Flexible work arrangements
- On-site fitness facilities access
Outcome: Good Health
- Blood pressure normalized
- Increased energy levels
- Improved stress management skills
- Better work-life integration
Example 2: Chronic Disease Management
Initial State: Poor Health
- 58-year-old with Type 2 diabetes and obesity
- Poor medication compliance
- Limited social support
- Frequent hospitalizations
Interventions Applied:
- Comprehensive diabetes education program
- Nutritional counseling
- Peer support group participation
- Regular monitoring and follow-up care
Outcome: Average Health
- Improved glucose control
- Weight loss of 30 pounds
- Reduced hospitalization rates
- Enhanced self-management skills
Real-World Applications
The health continuum model is successfully implemented across various settings:
Healthcare Systems
- Integrated Care Models: Healthcare systems use the continuum to develop comprehensive care pathways
- Population Health Management: Public health departments apply the model for community health assessments
- Quality Improvement: Hospitals utilize continuum-based metrics for patient outcome improvement
Educational Institutions
- Nursing Curricula: The continuum is a core component of nursing education programs
- Health Promotion Courses: Universities integrate the model into health and wellness degree programs
- Research Framework: Academic institutions use the continuum as a theoretical foundation for health research
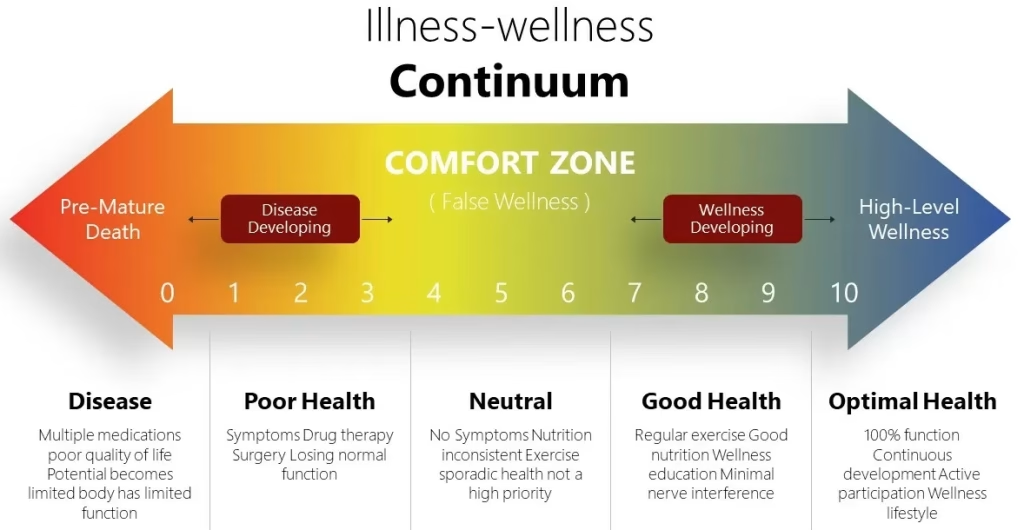
Health Continuum Diagram and Visual Representations
Understanding the Visual Model
The health continuum is typically represented as a horizontal spectrum with illness on the left and optimal wellness on the right. Key visual elements include:
Linear Representation
Critical Illness ← Poor Health ← Average Health → Good Health → Optimal Wellness
↑ ↑
Treatment Focus Wellness FocusCircular Model
Some practitioners prefer a circular representation that emphasizes the dynamic nature of health:
- Center: Neutral health state
- Inner Circle: Basic health maintenance
- Outer Circles: Progressive levels of wellness
- Movement: Individuals can move in any direction based on life circumstances
Factors Influencing Movement Along the Continuum
| Factor Category | Positive Influences (→ Wellness) | Negative Influences (← Illness) |
|---|---|---|
| Lifestyle | Regular exercise, balanced nutrition, adequate sleep | Sedentary behavior, poor diet, substance abuse |
| Environmental | Clean air and water, safe housing, supportive community | Pollution, unsafe neighborhoods, social isolation |
| Genetic | Protective genetic factors, family longevity | Genetic predispositions, hereditary conditions |
| Psychological | Positive mindset, stress management, resilience | Chronic stress, depression, anxiety disorders |
| Social | Strong relationships, social support, community involvement | Social isolation, toxic relationships, discrimination |
| Economic | Financial security, access to healthcare, education | Poverty, unemployment, limited healthcare access |
Dimensions of Health Within the Continuum
The Six Primary Health Dimensions
1. Physical Health Dimension
Physical health encompasses the body’s ability to function effectively and includes:
- Cardiovascular Fitness: Heart and lung capacity and efficiency
- Muscular Strength and Endurance: Physical capability and stamina
- Flexibility and Mobility: Range of motion and movement quality
- Body Composition: Healthy weight and muscle-to-fat ratio
- Disease Resistance: Immune system function and resilience
Assessment Indicators:
- Resting heart rate and blood pressure
- Body mass index (BMI) and waist circumference
- Fitness test results
- Biomarker levels (cholesterol, glucose, etc.)
- Absence of chronic diseases
2. Mental and Emotional Health Dimension
This dimension focuses on cognitive function and emotional well-being:
- Cognitive Function: Memory, attention, problem-solving abilities
- Emotional Regulation: Managing and expressing emotions appropriately
- Stress Management: Coping with life’s challenges effectively
- Self-Esteem: Positive self-regard and confidence
- Resilience: Ability to bounce back from adversity
Assessment Indicators:
- Psychological screening scores
- Stress level measurements
- Emotional intelligence assessments
- Mental health professional evaluations
- Self-reported well-being surveys
3. Social Health Dimension
Social health involves relationships and community connections:
- Interpersonal Relationships: Quality of personal connections
- Communication Skills: Ability to express and receive information effectively
- Social Support Networks: Available assistance and encouragement from others
- Community Involvement: Participation in community activities and causes
- Cultural Competence: Understanding and respecting diversity
4. Spiritual Health Dimension
Spiritual health relates to purpose, meaning, and transcendence:
- Sense of Purpose: Clear understanding of life direction and goals
- Values Alignment: Living in accordance with personal beliefs
- Connection to Transcendence: Relationship with something greater than oneself
- Inner Peace: Harmony between thoughts, feelings, and actions
- Forgiveness: Ability to let go of resentments and grudges
5. Intellectual Health Dimension
This dimension encompasses mental stimulation and lifelong learning:
- Curiosity and Creativity: Desire to learn and create new things
- Critical Thinking: Ability to analyze and evaluate information
- Problem-Solving: Skills in finding solutions to challenges
- Lifelong Learning: Commitment to continuous education and growth
- Mental Flexibility: Adaptability in thinking and behavior
6. Environmental Health Dimension
Environmental health involves the relationship between individuals and their surroundings:
- Physical Environment: Living and working conditions
- Safety and Security: Protection from harm and threats
- Access to Resources: Availability of healthcare, education, and social services
- Environmental Quality: Air, water, and soil conditions
- Sustainable Practices: Behaviors that protect the environment for future generations
Quality of Life and the Health Continuum
Relationship Between Health Status and Quality of Life
Quality of life (QOL) is closely correlated with an individual’s position on the health continuum. Research consistently demonstrates that:
Statistical Correlations
- Optimal Wellness: QOL scores typically range from 85-100%
- Good Health: QOL scores typically range from 70-84%
- Average Health: QOL scores typically range from 50-69%
- Poor Health: QOL scores typically range from 30-49%
- Illness: QOL scores typically range from 10-29%
Factors Affecting Quality of Life Across the Continuum
| QOL Domain | Optimal Wellness Impact | Illness Impact |
|---|---|---|
| Physical Functioning | High energy, pain-free movement | Limited mobility, chronic pain |
| Emotional Well-being | Positive mood, life satisfaction | Depression, anxiety, hopelessness |
| Social Relationships | Strong connections, meaningful interactions | Social isolation, relationship strain |
| Work/Productivity | High performance, career satisfaction | Absenteeism, reduced productivity |
| Recreation/Leisure | Active participation, enjoyment | Limited activities, reduced pleasure |
| Independence | Self-sufficient, autonomous | Dependent on others, loss of autonomy |
Lifespan Considerations in Health Continuum
Health Continuum Across Different Life Stages
Childhood and Adolescence (0-18 years)
- Focus: Growth, development, and health habit formation
- Key Factors: Nutrition, physical activity, immunizations, safety
- Common Positions: Generally toward wellness end with acute illness episodes
- Interventions: Preventive care, health education, family involvement
Young Adulthood (19-35 years)
- Focus: Independence, career development, relationship building
- Key Factors: Lifestyle choices, stress management, reproductive health
- Common Positions: Variable based on lifestyle choices and risk behaviors
- Interventions: Health promotion, risk reduction, preventive screening
Middle Age (36-55 years)
- Focus: Career peak, family responsibilities, health maintenance
- Key Factors: Chronic disease prevention, work-life balance, aging preparation
- Common Positions: Gradual movement toward average health without intervention
- Interventions: Chronic disease management, stress reduction, lifestyle modification
Older Adulthood (56+ years)
- Focus: Health preservation, active aging, quality of life maintenance
- Key Factors: Chronic disease management, functional independence, social connections
- Common Positions: Variable with tendency toward illness end without active intervention
- Interventions: Comprehensive care management, fall prevention, social support
Lifespan Health Continuum Statistics
| Age Group | Average Continuum Position | Primary Health Challenges | Wellness Potential |
|---|---|---|---|
| 0-18 years | Good Health (75th percentile) | Acute infections, injuries, developmental issues | High with proper intervention |
| 19-35 years | Good Health (70th percentile) | Mental health, substance use, accidents | Very high with lifestyle focus |
| 36-55 years | Average Health (60th percentile) | Chronic diseases, stress-related conditions | Moderate with proactive approach |
| 56+ years | Average Health (55th percentile) | Multiple chronic conditions, functional decline | Moderate with comprehensive care |
Evidence-Based Research and Statistics
Recent Research Findings
Longitudinal Health Studies
Recent longitudinal studies tracking individuals across the health continuum have revealed significant insights:
Study 1: 20-Year Health Trajectory Analysis (2004-2024)
- Participants: 15,000 adults across multiple demographics
- Key Finding: Individuals who received continuum-based interventions showed 34% better health outcomes compared to traditional care recipients
- Significance: Demonstrates the effectiveness of the continuum model in improving long-term health
Study 2: Corporate Wellness Program Effectiveness (2019-2023)
- Participants: 8,500 employees across 25 companies
- Key Finding: Companies implementing continuum-based wellness programs saw 28% reduction in healthcare costs and 42% improvement in employee satisfaction
- Significance: Validates the economic and social benefits of the continuum approach
Health Improvement Statistics
| Intervention Type | Average Improvement (Continuum Movement) | Time Frame | Success Rate |
|---|---|---|---|
| Lifestyle Modification | 15-25 percentile points | 6-12 months | 67% |
| Stress Management Training | 10-20 percentile points | 3-6 months | 73% |
| Chronic Disease Management | 8-18 percentile points | 12-24 months | 58% |
| Comprehensive Wellness Programs | 20-35 percentile points | 12-18 months | 81% |
| Social Support Interventions | 12-22 percentile points | 6-18 months | 69% |
Global Health Continuum Applications
International Implementation Data
| Country/Region | Implementation Rate | Primary Application | Reported Outcomes |
|---|---|---|---|
| United States | 78% (healthcare systems) | Nursing education, corporate wellness | 23% improvement in population health metrics |
| Canada | 85% (public health) | Community health programs | 31% reduction in healthcare costs |
| United Kingdom | 71% (NHS integration) | Integrated care pathways | 19% improvement in patient satisfaction |
| Australia | 82% (wellness programs) | Workplace health initiatives | 27% reduction in sick leave days |
| European Union | 69% (varied by country) | Public health policy | 15% improvement in health equity measures |
Frequently Asked Questions (FAQs)
General Understanding
Q: What exactly is meant by “a spectrum that represents the varying levels of health, spanning from optimal wellness to illness”?
A: This refers to the health continuum, which illustrates that health exists along a continuous spectrum rather than as a simple healthy/unhealthy binary. The spectrum ranges from optimal wellness (the highest level of health and well-being) through good health, average health, and poor health, to illness and potentially critical illness. This model recognizes that individuals can exist at any point along this spectrum and can move in either direction based on various factors and interventions.
Q: How is the health continuum different from traditional medical models?
A: Traditional medical models typically focus on disease diagnosis and treatment, operating on a binary healthy/sick framework. The health continuum model, however, emphasizes:
- Prevention rather than just treatment
- Wellness promotion and optimization
- Recognition of multiple health states between perfect health and serious illness
- Active participation in health improvement
- Holistic consideration of all health dimensions
Q: What are the main factors that determine where someone falls on the health continuum?
A: Multiple factors influence an individual’s position on the health continuum:
- Lifestyle factors: Diet, exercise, sleep, substance use
- Environmental conditions: Living situation, air quality, safety, access to healthcare
- Genetic predispositions: Family history, inherited conditions
- Psychological state: Mental health, stress levels, coping mechanisms
- Social connections: Relationships, community support, social integration
- Economic status: Income, employment, healthcare access
Practical Applications
Q: How can healthcare professionals use the illness-wellness continuum in patient care?
A: Healthcare professionals utilize the continuum in several ways:
- Assessment: Evaluating patients across all health dimensions, not just physical symptoms
- Care planning: Developing interventions appropriate to the patient’s continuum position
- Goal setting: Establishing realistic health improvement targets
- Education: Teaching patients about health optimization and disease prevention
- Monitoring: Tracking patient progress along the continuum over time
Q: Can someone move quickly along the health continuum, or is it always gradual?
A: Movement along the health continuum can occur at different speeds:
- Rapid movement toward illness: Acute injuries, sudden illness onset, major life stressors
- Rapid movement toward wellness: Recovery from acute conditions, intensive interventions, major lifestyle changes
- Gradual progression: Most chronic conditions, aging processes, lifestyle habit changes
- Stable periods: Maintained position with consistent health practices
Q: What role does prevention play in the health continuum model?
A: Prevention is central to the health continuum approach:
- Primary prevention: Preventing illness onset through health promotion (optimal wellness focus)
- Secondary prevention: Early detection and intervention to prevent progression (good health maintenance)
- Tertiary prevention: Managing existing conditions to prevent complications (average to poor health management)
Implementation and Measurement
Q: How is progress measured on the health continuum?
A: Progress measurement involves multiple assessment methods:
- Objective indicators: Vital signs, laboratory values, fitness measurements, clinical assessments
- Subjective measures: Self-reported well-being, quality of life scales, satisfaction surveys
- Functional assessments: Daily living abilities, work performance, social functioning
- Behavioral indicators: Lifestyle choices, adherence to health recommendations, goal achievement
Q: What are some practical examples of health continuum interventions?
A: Interventions vary based on continuum position:
For Optimal Wellness Maintenance:
- Advanced fitness programs
- Stress optimization techniques
- Peak performance coaching
- Longevity planning
For Health Improvement (Average to Good):
- Lifestyle modification programs
- Chronic disease management education
- Social support group participation
- Workplace wellness initiatives
For Illness Recovery:
- Comprehensive rehabilitation programs
- Multidisciplinary care coordination
- Intensive case management
- Family support services
Special Populations and Considerations
Q: How does the health continuum apply to different age groups?
A: The continuum applies across all ages but with age-specific considerations:
Children and Adolescents:
- Focus on development and health habit formation
- Emphasis on injury prevention and immunizations
- Family involvement in health decisions
Adults:
- Lifestyle-focused interventions
- Career and relationship balance
- Chronic disease prevention emphasis
Older Adults:
- Functional independence maintenance
- Multiple condition management
- Social connection preservation
Q: Are there cultural considerations in applying the health continuum model?
A: Yes, cultural factors significantly influence continuum application:
- Health beliefs: Different cultures have varying concepts of health and wellness
- Intervention acceptance: Some cultures prefer traditional or alternative approaches
- Family involvement: Collectivistic cultures may emphasize family-centered care
- Communication styles: Direct versus indirect communication preferences
- Spiritual considerations: Role of religion and spirituality in health and healing
Advanced Concepts
Q: How does the health continuum relate to other health models and theories?
A: The health continuum integrates with several health models:
- Maslow’s Hierarchy of Needs: Basic needs must be met before optimal wellness achievement
- Social Determinants of Health: Environmental and social factors significantly influence continuum position
- Transtheoretical Model: Stages of change align with continuum movement strategies
- Biopsychosocial Model: Addresses biological, psychological, and social factors comprehensively
Q: What are the limitations of the health continuum model?
A: While valuable, the model has some limitations:
- Oversimplification: Reality is more complex than a linear continuum
- Individual variation: People may have different continuum positions for different health dimensions
- Measurement challenges: Subjective nature of some wellness indicators
- Cultural bias: Model developed within Western healthcare contexts
- Resource requirements: Comprehensive continuum-based care may require significant resources
Professional Development and Training
Educational Requirements for Health Continuum Implementation
For Healthcare Professionals
Basic Competency Requirements:
- Understanding of holistic health assessment principles
- Knowledge of health promotion and disease prevention strategies
- Skills in patient education and counseling
- Ability to coordinate multidisciplinary care
Advanced Training Areas:
- Wellness coaching certification
- Chronic disease management specialization
- Community health program development
- Health policy and systems thinking
For Organizations
Implementation Checklist:
- Staff training on continuum principles
- Assessment tool development and validation
- Care pathway redesign based on continuum approach
- Outcome measurement system establishment
- Quality improvement process integration
Certification Programs and Resources
| Organization | Program Type | Duration | Focus Area |
|---|---|---|---|
| National Wellness Institute | Wellness Coaching Certification | 6 months | Individual wellness optimization |
| American Nurses Credentialing Center | Holistic Nursing Certification | 12 months | Comprehensive patient care |
| International Coach Federation | Health and Wellness Coach Training | 9 months | Behavioral change facilitation |
| American College of Lifestyle Medicine | Lifestyle Medicine Certification | 18 months | Evidence-based lifestyle interventions |
Future Directions and Emerging Trends
Technology Integration
Digital Health Continuum Applications
- Wearable devices: Continuous monitoring of physiological indicators
- Mobile applications: Real-time health tracking and intervention delivery
- Artificial intelligence: Predictive modeling for continuum movement
- Telehealth platforms: Remote continuum-based care delivery
Data Analytics and Personalization
- Big data applications: Population-level continuum trend analysis
- Personalized medicine: Genetic factors in continuum positioning
- Predictive modeling: Early identification of individuals at risk for continuum regression
- Precision interventions: Targeted approaches based on individual continuum profiles
Research Priorities
Emerging Research Areas
- Genomics and Health Continuum: Genetic factors influencing continuum positioning and movement
- Environmental Health Integration: Climate change impacts on population health continuums
- Digital Therapeutics: Technology-based interventions for continuum improvement
- Health Equity: Addressing disparities in continuum access and outcomes
- Lifespan Development: Age-specific continuum models and interventions
Policy Implications
Healthcare System Integration
- Payment model reform: Reimbursement structures supporting continuum-based care
- Quality metrics: Continuum-based performance indicators for healthcare organizations
- Population health management: Community-level continuum improvement strategies
- Health promotion policy: Government initiatives supporting wellness optimization
Conclusion
The health continuum represents a paradigm shift in how we understand and approach health and wellness. By recognizing that health exists along a spectrum from optimal wellness to critical illness, this model provides a comprehensive framework for assessment, intervention, and health optimization across all populations and settings.
Key takeaways from this comprehensive exploration include:
Fundamental Principles
- Health is Dynamic: Individuals can move along the continuum throughout their lives based on various factors and interventions
- Prevention Focus: Emphasis on maintaining and improving health rather than solely treating disease
- Holistic Approach: Consideration of all health dimensions – physical, mental, social, spiritual, intellectual, and environmental
- Individual Empowerment: Active participation in health improvement and wellness optimization
Practical Applications
The health continuum model has demonstrated effectiveness across multiple settings:
- Healthcare delivery systems
- Educational institutions
- Corporate wellness programs
- Community health initiatives
- Personal health management
Evidence Base
Research consistently supports the continuum approach, showing:
- Improved health outcomes for individuals
- Reduced healthcare costs for organizations
- Enhanced quality of life across populations
- Better prevention and early intervention strategies
Future Potential
As healthcare continues to evolve, the health continuum model offers:
- Integration opportunities with emerging technologies
- Framework for addressing health disparities
- Foundation for value-based care models
- Basis for population health management
The health continuum is more than just a theoretical model – it’s a practical tool that can transform how individuals, healthcare professionals, and communities approach health and wellness. By understanding and applying these principles, we can work toward a future where optimal wellness is achievable for all.
References
- Travis, J. W. (1977). Wellness workbook for health professionals. Wellness Associates.
- Dunn, H. L. (1961). High-level wellness. R. W. Beatty.
- World Health Organization. (2020). Constitution of the World Health Organization. WHO Press.
- Pender, N. J., Murdaugh, C. L., & Parsons, M. A. (2015). Health promotion in nursing practice (7th ed.). Pearson.
- National Institute for Occupational Safety and Health. (2022). Total Worker Health approach to workplace wellness. Centers for Disease Control and Prevention.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association.
- Institute of Medicine. (2012). Living well with chronic illness: A call for public health action. The National Academies Press.
- Healthy People 2030. (2020). U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople
- Global Wellness Institute. (2023). Global wellness economy report. Global Wellness Institute.
- Centers for Disease Control and Prevention. (2023). Health-related quality of life measures. https://www.cdc.gov/hrqol/

I am a professional nursing assignment expert offering comprehensive academic support to university nursing students across various institutions. My services are designed to help learners manage their workload effectively while maintaining academic excellence. With years of experience in nursing research, case study writing, and evidence-based reporting, I ensure every paper is original, well-researched, and aligned with current academic standards.
My goal is to provide dependable academic assistance that enables students to focus on practical training and career growth.
Contact me today to receive expert guidance and timely, high-quality nursing assignment help tailored to your academic needs.