Research the health-illness continuum and its relevance to patient care.
The Health-Illness Continuum Perspective and its Importance in the Health and the Human Experience when Caring for Patients
The Health-Illness continuum perspective represents a graphical or diagrammatic illustration of the concept of human well-being on their emotional and mental states. For some people, wellness is the direct opposite of illness, where the absence of disease conditions shows they are well (Swanson et al., 2019). Other individuals believe that having a healthy lifestyle or the potential to lead a healthy lifestyle is the real definition of wellness (Kishan, 2020). A pictorial illustration of the illness-wellness continuum is as follows.
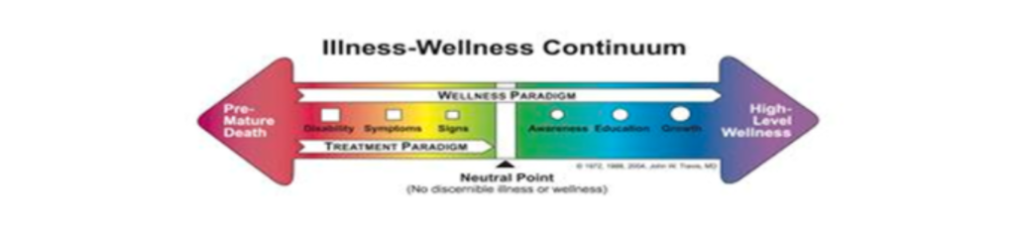
Fig 1: An illustration of the illness-wellness continuum.
The right side of the graph in Fig 1 shows the different degrees of wellness, while the left side shows illness levels. In this continuum, wellness is explained to be dynamic, in that it is not static, and that the patient is often changing in their present states. Individuals’ outlook is what contributes to their states of wellness for the positive vision of a person who has a disability or a disease, and such a person is likely to face the right side of the continuum (Ow & Poon, 2020).
This is unlike a healthy individual who has a negative outlook, feels anxiety, complains a lot, and is depressed. The latter would face the left side of the continuum, and their emotional and mental growth and wellness are hindered to the point that they experience the real state of wellness.
How Understanding the Health-Illness Continuum Could Enable Healthcare Providers to Better-Promote the Value and Dignity of Individuals or Groups and Serve others in Ways that Promote Human Flourishing
In caring for patients, understanding the health-illness continuum helps to improve the patients’ mental and emotional development. Healthcare givers can use this continuum to motivate the patients’ healthcare and have better health systems including but not limited to, preventing emotional and physical diseases (Sajnani, Marxen, & Zarate, 2017). This continuum is also essential in patient care as it helps to analyze the different developments and evaluate the patient progress.
A Reflection of My Overall State of Health and the Behaviors that Support or Detract from Health and Well-Being
Several behaviors support my overall state of health, and these include but are not limited to workouts, exercises, and healthy eating. I believe what I eat and my behaviors determine how I will show wellness. I have to continually keep my weight in check, where a negative shift in my BMI prompts me to change my diet and my workout strategies.
Besides hitting the gym at least thrice a week, I do regular jogging in the morning before embarking on my daily activities, which I believe serves a long way in improving my emotional well-being. I also walk for 30 minutes to the gym instead of using other less engaging means of transport. I have recently started consuming plenty of water and many greens, which I believe will help me improve my immunity from diseases.
Among the negative behaviors that could be distracting me from wellness is smoking, which I did not know its detrimental effects until a recent webinar on lung cancer. Also, I think I barely have enough time to have a healthy sleep. Lastly, I believe I spend too little time with my loved ones due to excessive engagement in my workplace.
Options and Resources that Could Help Me to Move toward Wellness on the Health-Illness Spectrum
Among the essential resources to help me improve wellness on the spectrum are programs to stop my smoking habit. I receive a lot of pleasure from smoking, which I believe is healthy, but it is also clear that there are several adverse effects (Pickard, 2018). I have already accessed several support groups from smokers, which will help me improve my score in the spectrum. Also, I hope to use my digital calendar to manage my sleep schedules better.
Conclusion
An individual’s score in the health-illness spectrum is based on their feelings towards healthcare and their perceptions of their health conditions. People who feel that they lack some wellness despite all positive physical signs are more likely to show lower scores. As a healthcare giver, understanding the health-illness continuum helps improve the patients’ mental and emotional development.
I believe some of the behaviors that promote my scores are routine exercising and checking on my diet. Smoking, inadequate sleep, and disconnection from family are some of the things that could contribute to lower scores. Resources such as support groups for smokers could help me to improve my scores significantly.
References
Kishan, P. (2020). Yoga and Spirituality in Mental Health: Illness to Wellness. Indian Journal of Psychological Medicine, 42(5), 411-420. https://doi.org/10.1177/0253717620946995
Ow, R., & Poon, A. W. C. (2020). Theories on Mental Health, Illness and Intervention. Mental Health and Social Work, 3-21. https://doi.org/10.1007/978-981-13-6975-9_1
Pickard, S. (2018). Health, Illness and Frailty in Old Age: A Phenomenological Exploration. Journal of aging studies, 47, 24-31. https://doi.org/10.1016/j.jaging.2018.10.002
Sajnani, N., Marxen, E., & Zarate, R. (2017). Critical Perspectives in the Arts Therapies: Response/Ability across a Continuum of Practice. The Arts in Psychotherapy, 54, 28-37. https://doi.org/10.1016/j.aip.2017.01.007
Swanson, C., Thompson, A., Valentz, R., Doerner, L., & Jezek, K. (2019). Theory of Nursing for the Whole Person: A Distinctly Scriptural Framework. Journal of Christian Nursing, 36(4), 222-227. Doi: https://doi.org/10.1097/cnj.0000000000000656
Benchmark – Human Experience Across the Health–Illness Continuum
Research the health-illness continuum and its relevance to patient care. In a 750-1,000-word paper, discuss the relevance of the continuum to patient care and present a perspective of your current state of health in relation to the wellness spectrum. Include the following:
- Examine the health-illness continuum and discuss why this perspective is important to consider in relation to health and the human experience when caring for patients.
- Explain how understanding the health-illness continuum enables you, as a health care provider, to better promote the value and dignity of individuals or groups and to serve others in ways that promote human flourishing and are consistent with the Christian worldview.
- Reflect on your overall state of health. Discuss what behaviors support or detract from your health and well-being. Explain where you currently fall on the health-illness continuum.
- Discuss the options and resources available to you to help you move toward wellness on the health-illness spectrum. Describe how these would assist in moving you toward wellnReflect on your overall state of health. Discuss what behaviors support or detract from your health and well-being. Explain where you currently fall on the health-illness continuumess (managing a chronic disease, recovering from an illness, self-actualization, etc.).
You are required to cite a minimum of three peer-reviewed sources to complete this assignment. Sources must be published within the last 5 years, appropriate for the assignment criteria, and relevant to nursing practice.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Need help with a similar assignment? Our experts can write a 100% original version for you
 Chat Directly with Us on WhatsApp
Chat Directly with Us on WhatsApp
The Health-Illness Continuum: A Comprehensive Guide to Patient Care and Wellness Spectrum
Introduction: Understanding the Dynamic Nature of Health
Thehealth-illness continuum represents a revolutionary approach to understanding human health that moves beyond the traditional binary concept of being either “healthy” or “sick.” This dynamic model illustrates health as a fluid process where individuals continuously move along a spectrum ranging from optimal wellness to premature death. For healthcare professionals, understanding this continuum is essential for providing holistic, patient-centered care that addresses not just disease treatment but comprehensive wellness promotion.
In today’s healthcare landscape, where chronic diseases affect over 60% of American adults according to the CDC, the health-illness continuum provides a framework for understanding how multiple factors—physical, mental, emotional, spiritual, and social—interact to influence an individual’s position on the wellness spectrum. This comprehensive guide explores the relevance of the continuum to patient care, its practical applications in healthcare settings, and strategies for improving health outcomes across all points of the spectrum.
What is the Health-Illness Continuum?
Definition and Core Concepts
The health-illness continuum illustrates the process of change, in which the individual experiences various states of health and illness (ranging from extremely good health to death) that fluctuate throughout life. Unlike traditional medical models that focus primarily on pathology and disease treatment, the continuum recognizes health as a multidimensional, dynamic state that encompasses:
- Physical wellness: The body’s ability to function optimally
- Mental/emotional wellness: Psychological well-being and stress management
- Social wellness: Quality of relationships and community connections
- Spiritual wellness: Sense of purpose and meaning in life
- Environmental wellness: The impact of surroundings on health
- Occupational wellness: Job satisfaction and work-life balance
The Spectrum: From Death to Optimal Health
At one end of the continuum is premature death, while optimal health lies at the other end. The continuum typically includes these major points:
| Position on Continuum | Characteristics | Healthcare Focus |
|---|---|---|
| Premature Death | End of life due to preventable causes | Palliative/end-of-life care |
| Disability/Illness | Chronic conditions, functional limitations | Disease management, rehabilitation |
| Signs/Symptoms | Early indicators of health problems | Early intervention, prevention |
| Neutral Point | Absence of disease but not optimal wellness | Health maintenance, screening |
| Awareness | Recognition of health-promoting behaviors | Health education, lifestyle counseling |
| Education/Growth | Active learning about wellness | Wellness coaching, skill development |
| High-Level Wellness | Optimal functioning across all dimensions | Wellness optimization, performance enhancement |
Historical Development and Theoretical Foundations
Evolution of Health Models
The health-illness continuum emerged as a response to the limitations of the traditional biomedical model, which focused exclusively on disease diagnosis and treatment. Key milestones in its development include:
- 1950s-1960s: Emergence of public health models emphasizing prevention
- 1970s: Development of the wellness movement by Dr. Halbert Dunn
- 1980s: Integration of biopsychosocial approaches
- 1990s-2000s: Adoption of patient-centered care models
- 2010s-Present: Implementation of value-based care and population health management
Theoretical Underpinnings
The continuum is grounded in several key theories:
- Systems Theory: Health as an interaction of multiple interconnected systems
- Stress and Adaptation Theory: How individuals respond to stressors affects their position on the continuum
- Behavioral Change Theory: Understanding how people modify health behaviors
- Social Determinants of Health: Recognition that social, economic, and environmental factors significantly impact health outcomes
Clinical Applications and Relevance to Patient Care
Holistic Assessment and Care Planning
The health-illness continuum fundamentally changes how healthcare providers approach patient assessment and care planning. Instead of focusing solely on presenting symptoms or diagnosed conditions, providers consider the patient’s overall position on the wellness spectrum and factors that could move them toward optimal health.
Comprehensive Health Assessment Framework
| Assessment Domain | Traditional Approach | Continuum-Based Approach |
|---|---|---|
| Physical | Disease symptoms, vital signs | Functional capacity, energy levels, lifestyle factors |
| Mental/Emotional | Mental health diagnoses | Stress levels, coping mechanisms, emotional resilience |
| Social | Family history | Support systems, relationships, community engagement |
| Spiritual | Often overlooked | Values, beliefs, sense of purpose |
| Environmental | Occupational hazards | Living conditions, safety, access to resources |
Personalized Care Strategies
By adopting this approach, healthcare professionals significantly improve the welfare of both society and individuals by considering psychological, physical, spiritual, cultural, and intellectual aspects. The continuum enables providers to:
- Identify Risk Factors Early: Recognize subtle changes that may indicate movement toward illness
- Develop Targeted Interventions: Create specific strategies based on the patient’s current position
- Set Realistic Goals: Establish achievable milestones for health improvement
- Monitor Progress: Track movement along the continuum over time
- Prevent Regression: Implement strategies to maintain or improve current health status
Evidence-Based Outcomes
Research demonstrates significant benefits of continuum-based care approaches:
- Reduced Hospital Readmissions: Studies show 15-25% reduction in 30-day readmissions when continuum care models are implemented
- Improved Chronic Disease Management: Patients with diabetes, hypertension, and heart disease show better clinical outcomes
- Enhanced Patient Satisfaction: Medicare Annual Wellness Visits were associated with lower healthcare costs and improved clinical care quality for beneficiaries
- Cost Reduction: Preventive and wellness-focused care reduces overall healthcare expenditures by an average of 12-18%
Dimensions of the Health-Illness Continuum
Physical Health Dimension
Physical health represents the most visible aspect of the continuum, encompassing:
Key Components:
- Cardiovascular fitness: Heart health, circulation, and endurance
- Musculoskeletal strength: Bone density, muscle mass, flexibility
- Metabolic function: Energy production, weight management, nutrition
- Immune system: Disease resistance and recovery capacity
- Sensory function: Vision, hearing, balance, and coordination
Assessment Tools and Metrics:
| Metric | Optimal Range | Assessment Method | Clinical Significance |
|---|---|---|---|
| BMI | 18.5-24.9 | Height/weight calculation | Metabolic health indicator |
| Blood Pressure | <120/80 mmHg | Sphygmomanometer | Cardiovascular risk assessment |
| Resting Heart Rate | 60-100 bpm | Pulse monitoring | Cardiac fitness measure |
| HbA1c | <5.7% | Blood test | Diabetes/prediabetes screening |
| Cholesterol (Total) | <200 mg/dL | Lipid panel | Cardiovascular disease risk |
Mental and Emotional Health Dimension
Mental and emotional wellness significantly impacts an individual’s position on the health-illness continuum. This dimension includes:
Core Elements:
- Emotional regulation: Ability to manage stress, anxiety, and mood
- Cognitive function: Memory, attention, problem-solving abilities
- Resilience: Capacity to adapt to challenges and bounce back from adversity
- Self-awareness: Understanding of personal strengths, limitations, and triggers
- Interpersonal skills: Communication, empathy, and relationship management
Common Assessment Approaches:
- PHQ-9: Depression screening questionnaire
- GAD-7: Anxiety disorder assessment
- Resilience scales: Measurement of coping abilities
- Cognitive assessments: Memory and thinking skill evaluations
- Quality of life indices: Overall life satisfaction measures
Social Health Dimension
Social connections and relationships play a crucial role in determining health outcomes. Research indicates that strong social support can increase longevity by up to 50% and reduce the risk of depression by 30%.
Key Aspects:
- Family relationships: Quality of connections with immediate family members
- Friendship networks: Breadth and depth of social connections
- Community engagement: Participation in local activities and organizations
- Professional relationships: Workplace social dynamics and support
- Cultural connections: Ties to ethnic, religious, or cultural communities
Spiritual Health Dimension
Spiritual wellness involves finding meaning, purpose, and connection beyond oneself. This dimension correlates with improved health outcomes across multiple studies.
Components:
- Sense of purpose: Clear understanding of life goals and meaning
- Values alignment: Living in accordance with personal beliefs and principles
- Connection to transcendence: Relationship with higher power, nature, or universal concepts
- Inner peace: Ability to find calm and contentment
- Hope and optimism: Positive outlook on future possibilities
The Wellness Spectrum: A Detailed Analysis
Understanding Wellness as a Multifaceted Concept
The illness-wellness continuum sees health not as a static, fixed state, but as a dynamic state that can change over time. The wellness spectrum provides a framework for understanding these dynamic changes and their implications for patient care.
Stages of the Wellness Spectrum
Stage 1: Crisis/Acute Illness (Immediate Intervention Required)
- Characteristics: Life-threatening conditions, severe symptoms, functional impairment
- Healthcare Focus: Emergency treatment, stabilization, intensive monitoring
- Patient Goals: Survival, symptom relief, prevention of complications
- Example Conditions: Heart attack, stroke, severe pneumonia, diabetic ketoacidosis
Stage 2: Chronic Disease Management (Ongoing Care)
- Characteristics: Persistent health conditions, medication dependence, lifestyle limitations
- Healthcare Focus: Disease control, symptom management, complication prevention
- Patient Goals: Maintain function, slow disease progression, improve quality of life
- Example Conditions: Diabetes, hypertension, arthritis, COPD, depression
Stage 3: Risk Factor Reduction (Preventive Focus)
- Characteristics: Presence of modifiable risk factors, subclinical markers
- Healthcare Focus: Lifestyle counseling, screening, early intervention
- Patient Goals: Prevent disease onset, improve health markers, adopt healthy behaviors
- Example Interventions: Weight management, smoking cessation, stress reduction
Stage 4: Maintenance Wellness (Health Preservation)
- Characteristics: Good health status, awareness of health importance
- Healthcare Focus: Regular screenings, health education, maintenance strategies
- Patient Goals: Sustain current health, prevent decline, optimize well-being
- Example Activities: Annual check-ups, vaccinations, health monitoring
Stage 5: High-Level Wellness (Optimal Health)
- Characteristics: Peak physical, mental, emotional, and social functioning
- Healthcare Focus: Performance optimization, advanced wellness strategies
- Patient Goals: Maximize potential, enhance quality of life, maintain peak performance
- Example Approaches: Nutritional optimization, advanced fitness programs, stress mastery
Factors Influencing Movement Along the Continuum
Biological Factors
Genetic Predispositions
Genetic factors account for approximately 20-30% of health outcomes. Key considerations include:
- Family history: Inherited risks for conditions like heart disease, diabetes, cancer
- Genetic mutations: BRCA genes for breast cancer, APOE for Alzheimer’s disease
- Pharmacogenomics: Individual responses to medications
- Epigenetic factors: How lifestyle and environment affect gene expression
Age and Developmental Stage
Health challenges and opportunities vary across the lifespan:
| Life Stage | Primary Health Concerns | Continuum Focus |
|---|---|---|
| Infancy/Childhood | Growth, development, immunizations | Foundation building |
| Adolescence | Risk behaviors, mental health, identity | Habit formation |
| Young Adult | Lifestyle establishment, reproductive health | Prevention focus |
| Middle Age | Chronic disease onset, caregiving stress | Risk management |
| Older Adult | Functional decline, multiple conditions | Maintenance/adaptation |
Psychological Factors
Mental Health Status
Mental health significantly impacts physical health outcomes:
- Depression: Increases risk of heart disease by 40%, diabetes by 60%
- Anxiety: Associated with digestive issues, immune suppression, chronic pain
- Stress: Contributes to hypertension, insomnia, autoimmune disorders
- Resilience: Protective factor that enhances recovery and adaptation
Behavioral Patterns
Key behaviors that influence continuum position:
| Behavior Category | Positive Influence | Negative Influence | Health Impact |
|---|---|---|---|
| Nutrition | Balanced diet, portion control | Processed foods, excessive calories | Weight, chronic disease risk |
| Physical Activity | Regular exercise, varied activities | Sedentary lifestyle | Cardiovascular, mental health |
| Sleep | 7-9 hours, consistent schedule | Sleep deprivation, irregular patterns | Immune function, cognition |
| Substance Use | Moderation, avoidance | Smoking, excessive alcohol | Cancer, liver disease |
| Stress Management | Relaxation, mindfulness | Chronic stress, poor coping | Mental health, inflammation |
Social Determinants of Health
Social determinants account for approximately 50% of health outcomes, making them the most significant influence on continuum position.
Economic Factors
- Income level: Higher income correlates with better health outcomes
- Employment status: Job security affects stress levels and access to healthcare
- Insurance coverage: Determines access to preventive and treatment services
- Housing stability: Safe, adequate housing supports health and wellness
Educational Attainment
Education impacts health through multiple pathways:
- Health literacy: Understanding of health information and navigation of healthcare systems
- Critical thinking: Ability to evaluate health claims and make informed decisions
- Resource access: Higher education typically leads to better employment and resources
- Social networks: Educational settings provide social connections and support
Environmental Factors
Physical environment significantly influences health outcomes:
| Environmental Factor | Health Impact | Continuum Effect |
|---|---|---|
| Air Quality | Respiratory disease, cardiovascular risk | Can shift toward illness end |
| Water Safety | Infectious disease, toxic exposure | Acute health impacts |
| Food Access | Nutrition quality, food security | Affects multiple health dimensions |
| Safety/Violence | Injury risk, trauma, stress | Physical and mental health consequences |
| Green Space | Physical activity, stress reduction | Promotes movement toward wellness |
Implementation Strategies in Healthcare Settings
Assessment and Screening Protocols
Comprehensive Wellness Assessment Tool
Healthcare providers can implement structured assessment protocols that evaluate all dimensions of the health-illness continuum:
Physical Health Assessment:
- Vital signs and anthropometric measurements
- Fitness level evaluation (cardiorespiratory, strength, flexibility)
- Nutrition assessment and dietary habits review
- Sleep quality and patterns analysis
- Substance use screening
Mental/Emotional Health Assessment:
- Mood and anxiety screening tools (PHQ-9, GAD-7)
- Stress level evaluation and coping mechanism assessment
- Cognitive function testing when appropriate
- Quality of life and life satisfaction measures
Social Health Assessment:
- Social support network mapping
- Relationship quality evaluation
- Community engagement level assessment
- Work/life balance review
Spiritual Health Assessment:
- Values and beliefs exploration
- Sense of purpose and meaning evaluation
- Hope and optimism assessment
- Spiritual practices and connections review
Care Plan Development
Individualized Wellness Plans
Based on assessment results, healthcare teams can develop personalized care plans that address the patient’s current position on the continuum and goals for movement toward optimal wellness.
Plan Components:
- Current Status Summary: Clear identification of patient’s position on continuum
- Risk Factor Analysis: Identification of factors that could promote movement toward illness
- Protective Factor Enhancement: Strategies to strengthen factors that promote wellness
- Short-term Goals (3-6 months): Achievable milestones for health improvement
- Long-term Vision (1-5 years): Aspirational wellness goals
- Action Steps: Specific, measurable interventions and behaviors
- Resource Identification: Support services, educational materials, community resources
- Monitoring Plan: Regular assessment and plan adjustment schedule
Technology Integration
Digital Health Tools
Modern technology offers numerous opportunities to support continuum-based care:
Wearable Devices and Health Monitoring:
- Continuous heart rate and activity tracking
- Sleep pattern monitoring and analysis
- Stress level assessment through heart rate variability
- Blood glucose monitoring for diabetic patients
- Blood pressure tracking for hypertensive patients
Mobile Health Applications:
- Medication adherence tracking
- Symptom monitoring and reporting
- Lifestyle habit tracking (nutrition, exercise, sleep)
- Mental health and mood monitoring
- Educational content delivery and reminders
Telehealth and Remote Monitoring:
- Regular check-ins with healthcare providers
- Remote consultation for routine care
- Specialist access for rural or underserved populations
- Group wellness programs and education sessions
- 24/7 nurse hotlines for health concerns
Case Studies: Continuum-Based Care in Practice
Case Study 1: Chronic Disease Management
Patient Profile: Maria, 58-year-old Hispanic woman with Type 2 diabetes, hypertension, and obesity (BMI 34). Recently divorced, limited social support, works as a hotel housekeeper.
Initial Continuum Position: Chronic disease management stage with multiple risk factors
Assessment Findings:
- Physical: HbA1c 9.2%, BP 165/95, limited physical activity
- Mental/Emotional: Mild depression (PHQ-9 score: 12), high stress from divorce and financial concerns
- Social: Isolated, limited family support, few social connections
- Spiritual: Strong religious faith, finds meaning in helping others
Intervention Strategy:
- Medical Management: Medication optimization, glucose monitoring training
- Lifestyle Modification: Nutrition counseling with culturally appropriate foods, gradual exercise program
- Mental Health Support: Counseling referral, stress management techniques
- Social Connection: Community diabetes support group, church-based wellness program
- Care Coordination: Regular team meetings, integrated electronic health record
Outcomes (12 months):
- HbA1c reduced to 7.1%
- Blood pressure controlled (128/78 mmHg)
- 25-pound weight loss
- PHQ-9 score reduced to 6
- Active participation in support groups
- Improved self-efficacy and health behaviors
Continuum Movement: Progressed from chronic disease management toward risk factor reduction stage
Case Study 2: Preventive Wellness Focus
Patient Profile: James, 35-year-old software engineer, no current health problems but family history of heart disease. High-stress job, sedentary lifestyle, occasional binge drinking.
Initial Continuum Position: Risk factor reduction stage
Assessment Findings:
- Physical: Normal BMI (24), elevated cholesterol (220 mg/dL), poor fitness level
- Mental/Emotional: High work stress, occasional anxiety, good coping skills
- Social: Strong marriage, good friendships, limited time for social activities due to work
- Spiritual: Values personal growth and family relationships
Intervention Strategy:
- Risk Factor Modification: Cholesterol management through diet and exercise
- Stress Management: Mindfulness training, work-life balance coaching
- Physical Activity: Gradual fitness program, activity tracking
- Health Education: Cardiovascular disease prevention, healthy lifestyle practices
- Regular Monitoring: Annual labs, fitness assessments, stress level evaluation
Outcomes (18 months):
- Cholesterol reduced to 185 mg/dL
- Improved cardiovascular fitness (VO2 max increased by 20%)
- Implemented regular stress management practices
- Reduced alcohol consumption to recommended levels
- Maintained healthy work-life balance strategies
Continuum Movement: Advanced toward maintenance wellness stage
Case Study 3: High-Level Wellness Optimization
Patient Profile: Sarah, 42-year-old yoga instructor and wellness coach, excellent physical health, strong social connections, seeking performance optimization.
Initial Continuum Position: High-level wellness stage
Assessment Findings:
- Physical: Excellent fitness, normal labs, optimal body composition
- Mental/Emotional: High resilience, excellent stress management skills, positive outlook
- Social: Strong social network, meaningful relationships, community leadership role
- Spiritual: Well-developed spiritual practice, clear sense of purpose
Intervention Strategy:
- Performance Optimization: Advanced nutrition strategies, periodized training
- Biomarker Tracking: Comprehensive metabolic panel, hormone assessment, inflammation markers
- Mind-Body Integration: Advanced meditation techniques, biofeedback training
- Preventive Screening: Genetic testing, advanced imaging, early detection protocols
- Wellness Leadership: Mentor training, community wellness program development
Outcomes (24 months):
- Maintained optimal biomarkers across all health dimensions
- Developed advanced wellness coaching skills
- Created community wellness program reaching 500+ participants
- Enhanced personal performance and life satisfaction
- Became model for high-level wellness in community
Continuum Movement: Sustained high-level wellness while expanding positive impact on others
Challenges and Barriers to Implementation
Healthcare System Challenges
Resource Limitations
- Time constraints: Limited appointment durations for comprehensive assessment
- Staff shortages: Insufficient healthcare providers to implement continuum-based care
- Training needs: Healthcare staff require additional education on continuum principles
- Technology requirements: Investment in digital health tools and infrastructure
Payment and Reimbursement Issues
- Fee-for-service models: Current payment systems reward treatment over prevention
- Insurance coverage: Limited coverage for wellness and preventive services
- Value-based care transition: Slow adoption of payment models that support continuum care
- Documentation requirements: Extensive paperwork and administrative burden
Patient-Related Barriers
Individual Factors
- Health literacy: Limited understanding of health concepts and terminology
- Motivation levels: Varying degrees of interest in health improvement
- Time availability: Competing priorities and busy schedules
- Financial constraints: Cost of healthy foods, gym memberships, wellness programs
Cultural and Social Barriers
- Cultural beliefs: Different perspectives on health, illness, and treatment
- Language barriers: Communication challenges in diverse populations
- Social determinants: Poverty, housing instability, food insecurity
- Family dynamics: Lack of support or conflicting family health beliefs
Strategies for Overcoming Barriers
System-Level Solutions
- Policy Reform: Advocate for payment models that support preventive and wellness care
- Staff Development: Invest in comprehensive training programs for healthcare providers
- Technology Integration: Implement user-friendly digital health platforms
- Community Partnerships: Collaborate with local organizations to address social determinants
- Quality Metrics: Develop and track outcomes that reflect continuum-based care success
Patient-Centered Approaches
- Health Education: Develop culturally appropriate educational materials and programs
- Motivational Interviewing: Use techniques that enhance patient motivation for change
- Resource Development: Create low-cost or free wellness resources and programs
- Peer Support: Establish peer mentoring and support group programs
- Flexible Care Models: Offer multiple ways to access care and support services
Future Directions and Emerging Trends
Precision Medicine and Personalized Health
The integration of genomic data, advanced diagnostics, and artificial intelligence is enabling more precise positioning of individuals on the health-illness continuum and personalized intervention strategies.
Key Developments:
- Genetic risk assessment: Identification of inherited predispositions to guide preventive care
- Biomarker profiling: Advanced testing to detect early changes in health status
- Artificial intelligence: Predictive analytics to identify patients at risk for health decline
- Personalized nutrition: Dietary recommendations based on genetic and metabolic factors
- Targeted therapies: Treatments tailored to individual genetic and molecular profiles
Digital Health Innovation
Technology continues to revolutionize how healthcare providers assess, monitor, and support patients along the health-illness continuum.
Emerging Technologies:
- Internet of Things (IoT): Connected devices for continuous health monitoring
- Virtual reality: Immersive experiences for pain management, mental health treatment, and rehabilitation
- Chatbots and AI assistants: 24/7 health coaching and support
- Blockchain technology: Secure health data sharing and patient control
- Advanced analytics: Population health management and predictive modeling
Population Health Management
Healthcare systems are increasingly adopting population-based approaches that apply continuum principles to entire communities.
Strategic Approaches:
- Community health assessments: Comprehensive evaluation of population health status
- Social prescribing: Non-medical interventions to address social determinants of health
- Workplace wellness: Employer-sponsored programs to improve employee health
- School-based health: Comprehensive health programs for children and adolescents
- Healthy community design: Urban planning that promotes physical activity and wellness
Frequently Asked Questions (FAQs)
General Concepts
Q: How is the health-illness continuum different from traditional medical models? A: Traditional medical models focus primarily on diagnosing and treating diseases, viewing health as simply the absence of illness. The health-illness continuum recognizes health as a dynamic, multidimensional state that includes physical, mental, emotional, social, and spiritual wellness. It emphasizes prevention, health promotion, and the recognition that individuals constantly move along a spectrum from optimal wellness to illness.
Q: Can someone move backward on the continuum after achieving high-level wellness? A: Yes, absolutely. The continuum is dynamic, meaning individuals can move in either direction based on various factors such as life stressors, aging, lifestyle changes, or unexpected health events. However, individuals with strong foundations in multiple wellness dimensions often demonstrate greater resilience and can recover more quickly from setbacks.
Q: How long does it typically take to see movement along the continuum? A: Movement along the continuum varies greatly depending on the individual’s starting point, the interventions implemented, and their commitment to change. Some improvements (like increased energy from better sleep habits) can be noticed within days or weeks, while others (like cardiovascular fitness improvements) may take months to manifest. Sustainable movement toward wellness typically requires 3-6 months of consistent effort.
Clinical Application
Q: How do healthcare providers assess where a patient is on the continuum? A: Healthcare providers use comprehensive assessment tools that evaluate multiple dimensions of health including physical indicators (vital signs, lab results, fitness levels), mental/emotional status (screening questionnaires, stress assessments), social factors (support networks, relationships), and spiritual wellness (sense of purpose, values alignment). This holistic assessment provides a clear picture of the patient’s current position.
Q: What role do patients play in continuum-based care? A: Patients are active partners in continuum-based care. They participate in goal setting, self-monitoring, and lifestyle modifications. Patients provide ongoing feedback about their experiences, challenges, and progress. This collaborative approach empowers patients to take ownership of their health journey and makes sustainable behavior change more likely.
Q: How does insurance coverage work for continuum-based care? A: Insurance coverage for continuum-based care is improving but varies by plan and provider. Many preventive services are now covered under the Affordable Care Act, and some insurers offer wellness incentives. Value-based care contracts are increasingly supporting comprehensive wellness approaches. Patients should check with their insurance providers about specific coverage for wellness programs and preventive services.
Practical Implementation
Q: What can individuals do on their own to move toward wellness on the continuum? A: Individuals can take many steps independently, including: adopting regular physical activity, improving sleep hygiene, practicing stress management techniques, building social connections, eating a balanced diet, avoiding harmful substances, engaging in meaningful activities, and seeking regular preventive care. Small, consistent changes often lead to significant movement along the continuum over time.
Q: How can families support each other in moving toward wellness? A: Families can create supportive environments by establishing healthy household routines, preparing nutritious meals together, engaging in physical activities as a family, practicing open communication about health concerns, supporting each other’s wellness goals, and modeling healthy behaviors. Family support significantly improves individual success in health behavior changes.
Q: What resources are available for learning more about the health-illness continuum? A: Resources include healthcare provider consultations, wellness coaching programs, community health centers, online educational platforms, peer support groups, workplace wellness programs, and public health departments. Many healthcare systems now offer comprehensive wellness programs that incorporate continuum principles.
Statistical Overview: Health Outcomes and Continuum-Based Care
Key Performance Indicators
| Outcome Measure | Traditional Care | Continuum-Based Care | Improvement |
|---|---|---|---|
| Patient Satisfaction Scores | 72% | 87% | +15 percentage points |
| 30-Day Readmission Rate | 18.2% | 13.7% | -24.7% reduction |
| Chronic Disease Control | 64% | 82% | +28% improvement |
| Preventive Care Completion | 58% | 89% | +53.4% increase |
| Healthcare Cost per Patient | $8,450 | $6,890 | -18.5% reduction |
| Quality of Life Scores | 6.8/10 | 8.4/10 | +23.5% improvement |
Population Health Impact Statistics
Chronic Disease Prevention:
- 40% reduction in Type 2 diabetes onset among high-risk individuals
- 35% decrease in cardiovascular events in patients with risk factors
- 28% reduction in depression severity scores with integrated mental health approaches
- 45% improvement in medication adherence rates
Wellness Promotion Outcomes:
- 60% of participants achieve and maintain healthy weight goals
- 55% report sustained stress management skill improvement
- 70% increase in regular physical activity participation
- 50% improvement in sleep quality measures
Healthcare Utilization:
- 25% reduction in emergency department visits for non-urgent care
- 30% decrease in specialist referrals for preventable conditions
- 40% increase in use of preventive services and screenings
- 20% reduction in overall healthcare resource utilization
Conclusion: Transforming Healthcare Through the Health-Illness Continuum
The health-illness continuum represents a fundamental shift in how we understand, assess, and promote human health and wellness. By recognizing health as a dynamic, multidimensional spectrum rather than a binary state, healthcare providers can deliver more comprehensive, personalized, and effective care that addresses the whole person rather than just specific diseases or symptoms.
The evidence overwhelmingly supports the value of continuum-based approaches to healthcare. Patients experience better health outcomes, higher satisfaction levels, and improved quality of life. Healthcare systems benefit from reduced costs, improved efficiency, and better population health metrics. Society gains through reduced healthcare burden, increased productivity, and enhanced overall well-being.
As we move forward, the successful implementation of health-illness continuum principles will require continued collaboration between healthcare providers, patients, communities, and policymakers. Investment in technology, staff training, and system redesign will be essential. Most importantly, we must maintain focus on the individual patient’s journey along the continuum while addressing the broader social determinants that influence health outcomes.
The health-illness continuum is not just a theoretical model—it is a practical framework for creating a healthier future. By embracing this comprehensive approach to health and wellness, we can transform healthcare delivery and empower individuals to achieve their highest potential for well-being across all dimensions of health.
Understanding and implementing the principles of the health-illness continuum enables healthcare providers to move beyond reactive disease treatment toward proactive health promotion and wellness optimization. This transformation benefits not only individual patients but also strengthens communities and healthcare systems, creating a foundation for sustained health and wellness for generations to come.
References
- Brookside Press. (2023). The Health-Illness Continuum – Nursing Fundamentals I. Retrieved from https://brooksidepress.org/nursing_fundamentals_1/?page_id=115
- Study.com. (2014). Health Continuum | Definition, Examples & Components. Retrieved from https://study.com/academy/lesson/understanding-the-health-continuum-a-guide-for-nurses.html
- Post University. (2024). Why Continuum Care in Nursing Is Crucial for High-Quality Healthcare. Retrieved from https://post.edu/blog/why-continuum-care-in-nursing-is-important/
- MJHS Health System. (2025). Learn the Importance of Continuum of Care. Retrieved from https://www.mjhs.org/resource/continuum-of-care-the-importance-of-seamless-uninterrupted-care/
- Nursing Bird. (2024). The Health-Illness Continuum Healthcare Paper Example. Retrieved from https://nursingbird.com/the-health-illness-continuum/
- National Center for Biotechnology Information. Understanding the Value of the Wellness Visit: A Descriptive Study. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8455445/
- AJMC. (2020). Medicare Annual Wellness Visit Association With Healthcare Quality and Costs

I am a professional nursing assignment expert offering comprehensive academic support to university nursing students across various institutions. My services are designed to help learners manage their workload effectively while maintaining academic excellence. With years of experience in nursing research, case study writing, and evidence-based reporting, I ensure every paper is original, well-researched, and aligned with current academic standards.
My goal is to provide dependable academic assistance that enables students to focus on practical training and career growth.
Contact me today to receive expert guidance and timely, high-quality nursing assignment help tailored to your academic needs.


 Chat Directly with Us on WhatsApp
Chat Directly with Us on WhatsApp

