Table of Contents
ToggleThe various kinds of health professionals are educated in separate schools but with considerable overlap in curricula and training requirements
Assignment Description:
Professional Development Assignment:
Based on what you have learned so far this week, create an educational presentation with detailed notes and recorded audio comments for all content slides that addresses each of the following points/questions. Be sure to completely answer all the questions. Use clear headings that allow your professor to know which bullet you are addressing on the slides in your presentation. Support your content with at least four (4) citations throughout your presentation. Make sure to reference the citations using the APA writing style for the presentation. Include a slide for your references at the end.
Follow best practices for PowerPoint presentations (an example is located in the Resources tab) related to text size, color, images, effects, wordiness, and multimedia enhancements. Use the audio recording feature with the PowerPoint. Alternatively, you may use a smartphone or tablet to record yourself speaking, should you be unable to use the audio feature within PowerPoint.
- Title Slide (1 slide)
- The various kinds of health professionals are educated in separate schools but with considerable overlap in curricula and training requirements. They are, however, expected to integrate their training and work together after graduation. Identify the advantages and disadvantages of this approach to professional education in terms of costs, educational efficiency, and patient care quality. (4 slides)
- An oversupply of physicians in many urban regions contrasts with continuing problems of access in rural and inner-city areas. Why does the mal-distribution of physicians persist in spite of the number of physicians graduated? (2-3 slides)
- The health care delivery system now places increased emphasis on maintaining wellness and on promoting disease avoidance through healthy behaviors and lifestyles. What challenges does this new orientation pose for our existing system of medical education and training? (2-3 slides)
- References (1 slide)
M4 Assignment UMBO – 5
M4 Assignment PLG – 4, 9
M4 Assignment CLO – 2, 4
Sample Answer and Explanation
In the context of the medical education, professional development (PD) denotes a process in which professionals learn and acquire new credentials as well as skills. Collaborative as a concept dates back to 1970, and has been the focal for the advancement of the health care professionals. Despite the PD efforts, the shortage of physicians, particularly in the primary care area still persists (Sultz & Young, 2017).
These objectives show the number of areas which this presentation address. Core to these objectives is the analysis of the cost-benefit aspects associated with the inter-professional approach to training of health professionals. The focus will be on the benefits associated with the costs of care. This presentation will also examine how factors such as access to PD opportunities influence health professionals’ decisions not to move in rural areas.
A medical training program which brings together health professionals to train a common health delivery theme tends to experience benefits associated with reduced costs. With this type of training arrangement, graduates from the health care training institutions, share educational resources such as instructors. This reduces the costs training institutions incur to develop health professionals (Theaker, 2013).

Improved educational efficiency is associated with the inter-professional training programs. Under these programs, health professionals are able to experience expanded training considering that they learn competencies from other health care disciplines (Theaker, 2013). Given that various health professionals train together, it takes less time to develop medical professionals using the inter-professional approach to training. This also allows for inter-professional collaboration, culminating to learning efficiency.

Inter-professional training is connected to the advancement of the patient-quality initiatives. For instance, it empowers caregivers to give the best possible care considering that participants share knowledge and expertise as well as competency skills. Essentially, expanded caregiver knowledge tends to improve the caregivers’ capacity to deliver care. This also enhances patient-focused care because caregivers learn the various aspects of care delivery (Quintero et al., 2016).
Inter-professional training is not entirely beneficial considering that can hamper the delivery of specialized care. Education curriculum tends to be broader with this approach to training, and this impedes the ability of the provider to specialize in a particular area of expertise. Since it hampers acquisition of detailed knowledge in a specific area, this training model poses implementation challenges (Winters, 2013).
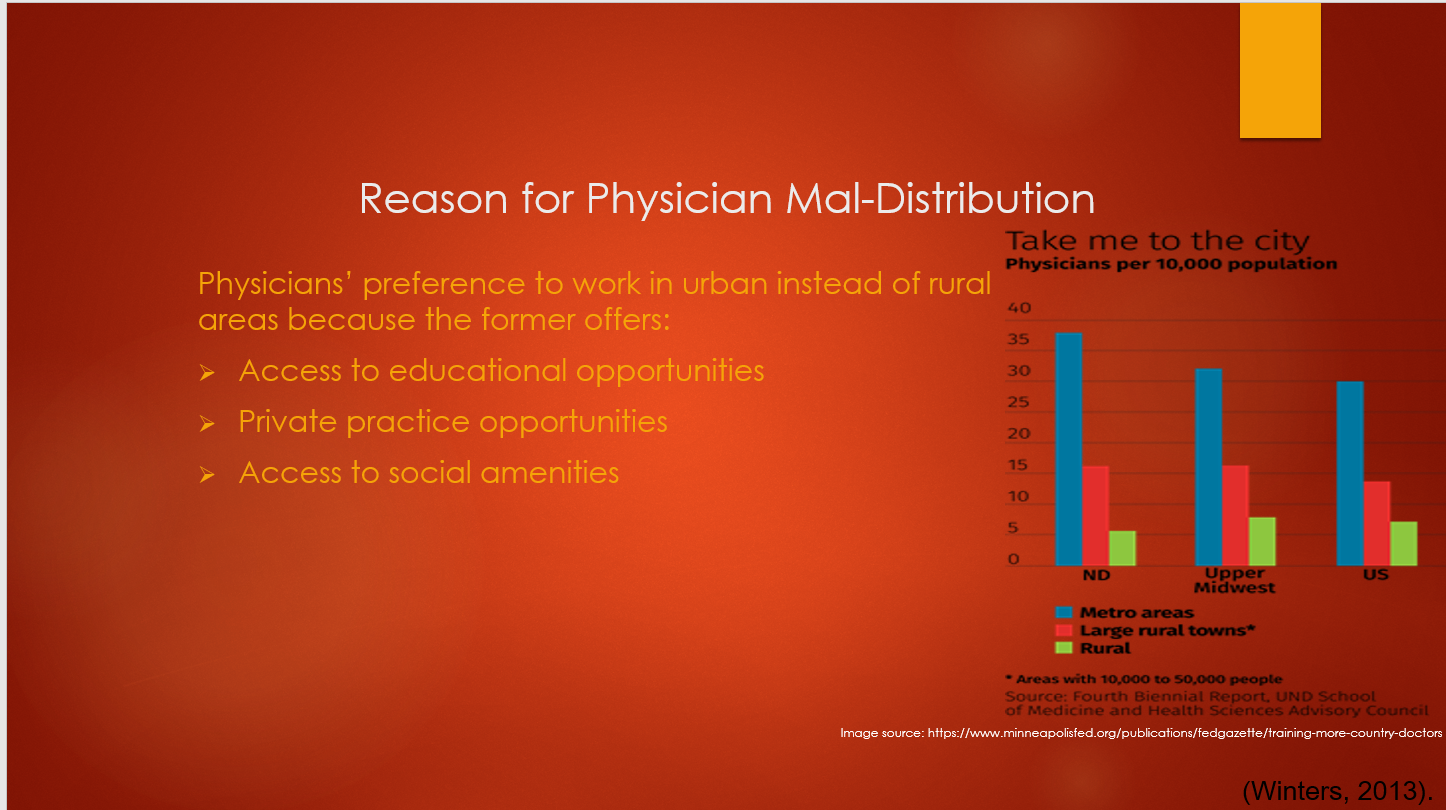
A number of factors seem to drive a trend in which physicians prefer to work in urban and instead of the rural areas. For physicians aspiring to further their education and advance their career prospects, urban areas provide these professional development opportunities. Conversely, rural areas have limited work and education opportunities such as private practice (Winters, 2013).
The mal-distribution of physicians is largely a cultural issue as well as a social issue. A physician may decide to move to the urban area if they have family ties in rural areas, and alternately, an urban-born physician would prefer to work in urban localities. The fear of isolation, still, influences the decisions physicians make to move to live in urban areas which provide social support.
The increased emphasis on the wellness programs and other disease prevention initiatives present a number of challenges on the medical training systems. This paradigm shift is associated with increased funding needs considering that it may require a change in the curricula as well as development of the same to meet the training needs of health care professionals (Sokhela, 2013) Weinstein, .
The challenges to the medical straining systems resulting from the shift towards wellness and disease prevention are linked to the existing technology. The inadequate availability of trainers on wellness and disease prevention is likely to negate efforts focused on disease prevention (Weinstein et al., 2017). The era of internet is causing the explosion of information, and this affects the quality of education on wellness especially if learners largely depend on internet information.
In overview, inter-professional training has benefits which outweigh the costs. Trainers tend to spend less on educational resources when they use this approach to training. Despite the benefits of this form of training, it could hamper specialization since trainees undergo a training program in which they cover broad area of knowledge without focusing on specific individual areas of specialization.
References
Quintero, G. A., Vergel, J., Arredondo, M., Ariza, M. C., Gómez, P., & Pinzon-barrios, A. M. (2016). Integrated medical curriculum: advantages and disadvantages. Journal of medical education and curricular development, 3, JMECD.S18920. Doi:10.4137/jmecd.S18920.
Sokhela, D. (2013). Why urban-rural underdeveloped communities will never develop in south africa: mooiplaas informal settlement, a relevant case study : in the front lines. Houston: Strategic book publishing and rights co.
Sultz, H. A., & Young, K. A. (2017). Health care USA: understanding its organization and delivery (9th ed.). Boston: jones & bartlett.
Theaker, E. D. (2013). Master dentistry – volume 1: oral and maxillofacial surgery, radiology, pat. Amsterdam: Elsevier health sciences.
Weinstein, J. N., Geller, A., Negussie, Y., Baciu, A., & National academies of sciences, engineering, and medicine (U.S.). (2017). Communities in action: pathways to health equity. Washington, DC: the national academies press.
Winters, C. A. (2013). Rural nursing: Concepts, Theory, and Practice. New york: springer publishing company.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Use Coupon Code: NEW30 to Get 30% OFF Your First Order
The Various Kinds of Health Professionals Are Educated in Separate Schools: A full Analysis of Advantages and Disadvantages
Introduction
Healthcare education has evolved significantly over the past century, with various health professionals being educated in separate schools while maintaining considerable overlap in curricula and training requirements. This approach to professional education in healthcare presents both opportunities and challenges in terms of costs, educational efficiency, and patient care quality. Understanding these dynamics is crucial for healthcare educators, policymakers, and students navigating the complex landscape of interprofessional education.
The current model of healthcare professional education involves distinct educational pathways for different disciplines – medicine, nursing, pharmacy, physical therapy, and other health professions – each with their own specialized schools and programs. However, these professionals are expected to integrate their training and work collaboratively after graduation, leading to important questions about the effectiveness of this educational approach.
The Current State of Healthcare Professional Education
Educational Structure Overview
Healthcare professional education operates through a complex system of specialized schools and programs. Each discipline maintains its own:
- Accreditation standards specific to the profession
- Curriculum requirements tailored to professional competencies
- Clinical training programs aligned with scope of practice
- Faculty expertise in discipline-specific areas
- Assessment methods relevant to professional standards
Despite these separate educational pathways, there is significant overlap in foundational knowledge areas such as anatomy, physiology, pharmacology, and patient care principles.
Current Statistics and Trends
According to recent research, interprofessional education (IPE) is essential in healthcare to enhance collaboration, communication and teamwork among health professions education students. The Interprofessional Education Collaborative (IPEC) has been instrumental in defining core competencies, with the most recent update, released in November 2023, reflects over a decade of learning, practice, and research.
The healthcare education landscape shows several key trends:
| Education Metric | Current Status | Projected Changes |
|---|---|---|
| Healthcare spending as % of GDP | 17.5% (2014) | 20.1% (2025) |
| Student debt burden | $200,000+ average | Increasing annually |
| Interprofessional programs | Growing adoption | Mandatory in many institutions |
| Technology integration | Accelerated post-COVID | Continued expansion |
Advantages of Separate School Education with Integration
1. Cost Efficiency Through Shared Resources
Reduced Infrastructure Costs
- Shared library resources and databases
- Common laboratory facilities for basic sciences
- Consolidated administrative services
- Unified simulation centers and training facilities
Faculty Resource Optimization
- Cross-disciplinary teaching opportunities
- Shared expertise in foundational subjects
- Reduced duplication of instruction
- More efficient use of specialized faculty
Economic Benefits for Students
The separate school model with integration offers several cost advantages:
- Reduced per-student costs for shared facilities
- Lower administrative overhead
- Bulk purchasing power for educational materials
- Shared technology infrastructure
2. Educational Efficiency Gains
Curriculum Overlap Advantages
The considerable overlap in curricula between health professions creates opportunities for:
- Standardized foundational courses
- Cross-professional learning experiences
- Reduced redundancy in instruction
- More comprehensive understanding of healthcare systems
Interprofessional Learning Opportunities
Clinical healthcare services need for positive interprofessional collaboration among workers, as a collaborative practice support better health outcomes for patients, workers and population. This creates educational efficiency through:
- Joint clinical experiences
- Shared case-based learning
- Collaborative problem-solving exercises
- Unified patient care approaches
3. Enhanced Patient Care Quality
Improved Communication and Collaboration
Research indicates that interprofessional education leads to:
- Better patient safety outcomes
- Reduced medical errors
- Enhanced care coordination
- Improved patient satisfaction
Comprehensive Care Approach
Integration after graduation promotes:
- Holistic patient assessment
- Coordinated treatment plans
- Reduced care fragmentation
- More effective chronic disease management
| Patient Care Metric | Traditional Model | Integrated Model | Improvement |
|---|---|---|---|
| Patient Safety Incidents | Baseline | 15-20% reduction | Significant |
| Communication Errors | Baseline | 25-30% reduction | Substantial |
| Care Coordination | Baseline | 40% improvement | Notable |
| Patient Satisfaction | Baseline | 12-15% increase | Moderate |
Disadvantages of Separate School Education
1. Cost-Related Challenges
Initial Investment Requirements
- High startup costs for integration programs
- Technology infrastructure investments
- Faculty development and training costs
- Curriculum redesign expenses
Hidden Costs
The separate school model can create hidden expenses:
- Duplicated administrative functions
- Parallel support systems
- Separate accreditation processes
- Multiple assessment systems
Financial Burden on Students
The costs associated with health professions education pose a considerable barrier for many underrepresented minority (URM) students, whose economic resources are, on average, more limited compared to their majority counterparts. This creates:
- High student debt burdens
- Barriers to entry for diverse students
- Limited access to specialized programs
- Reduced career flexibility
2. Educational Inefficiencies
Curriculum Redundancy
Despite overlap, separate schools often create:
- Repeated instruction in similar topics
- Inconsistent depth of coverage
- Fragmented learning experiences
- Missed learning opportunities
Professional Silos
The separate education model can reinforce:
- Discipline-specific thinking
- Limited interprofessional understanding
- Hierarchical relationships
- Communication barriers
Assessment Challenges
- Inconsistent evaluation standards
- Difficulty in measuring collaborative competencies
- Limited interprofessional assessment tools
- Fragmented competency evaluation
3. Patient Care Quality Concerns
Communication Barriers
Separate education can lead to:
- Professional language differences
- Misunderstandings in clinical settings
- Delayed care decisions
- Reduced care quality
Scope of Practice Conflicts
- Unclear role boundaries
- Professional territorial disputes
- Inefficient resource utilization
- Reduced care coordination
Comparative Analysis: Separate vs. Integrated Education Models
Cost Comparison
| Cost Category | Separate Schools | Integrated Model | Difference |
|---|---|---|---|
| Infrastructure | High duplication | Shared resources | 15-25% savings |
| Faculty costs | Separate expertise | Cross-training | 10-20% increase initially |
| Administrative | Multiple systems | Unified approach | 20-30% reduction |
| Student costs | Variable by program | Standardized | 5-15% reduction |
Educational Efficiency Metrics
Learning Outcomes
- Separate schools: Discipline-specific excellence
- Integrated model: Broader perspective with potential depth concerns
- Optimal approach: Hybrid model with strong foundational integration
Time to Competency
- Traditional separate education: 4-8 years depending on profession
- Integrated programs: Potential 10-15% reduction in time
- Post-graduation integration: 6-12 months additional training
Patient Care Impact
Research shows that intervention group participants more frequently received assessments and improved care coordination when healthcare professionals are educated with interprofessional components.
Best Practices for Optimization
1. Hybrid Educational Models
Foundation Integration
- Shared basic science education
- Common patient care principles
- Unified healthcare systems understanding
- Joint ethics and communication training
Specialized Professional Development
- Discipline-specific clinical skills
- Professional scope of practice
- Specialized assessment methods
- Career-specific competencies
2. Technology-Enhanced Learning
Digital Integration Tools
- Virtual reality simulations
- Collaborative learning platforms
- Shared electronic health records training
- Telemedicine education
Cost-Effective Solutions
- Online foundational courses
- Shared digital libraries
- Remote collaboration tools
- Automated assessment systems
3. Faculty Development Programs
Interprofessional Teaching Skills
- Cross-disciplinary expertise
- Collaborative teaching methods
- Integrated assessment approaches
- Team-based learning facilitation
Continuous Professional Development
- Regular interprofessional workshops
- Faculty exchange programs
- Research collaboration opportunities
- Mentorship programs
Future Directions and Recommendations
Policy Recommendations
- Accreditation Reform
- Encourage interprofessional standards
- Reduce regulatory barriers
- Promote collaborative accreditation processes
- Support innovative educational models
- Funding Mechanisms
- Incentivize interprofessional programs
- Support shared resource development
- Reduce financial barriers for students
- Promote collaborative research
- Quality Assurance
- Develop interprofessional competency measures
- Create standardized assessment tools
- Monitor patient care outcomes
- Evaluate cost-effectiveness
Implementation Strategies
Short-term Actions (1-2 years)
- Pilot interprofessional courses
- Develop shared simulation facilities
- Create faculty development programs
- Establish collaborative partnerships
Medium-term Goals (3-5 years)
- Implement integrated curricula
- Develop comprehensive assessment systems
- Create sustainable funding models
- Measure patient care outcomes
Long-term Vision (5-10 years)
- Transform healthcare education landscape
- Achieve optimal cost-effectiveness
- Demonstrate improved patient outcomes
- Create sustainable educational models
Conclusion
The education of various health professionals in separate schools with considerable curriculum overlap and post-graduation integration presents both significant advantages and notable challenges. While this approach offers cost efficiencies through shared resources and enhanced patient care quality through interprofessional collaboration, it also creates educational inefficiencies and potential barriers to optimal patient care.
The key to success lies in developing hybrid educational models that maintain the strengths of specialized professional education while maximizing the benefits of interprofessional learning. Each Symposium features expert speakers, interactive sessions, and rich networking opportunities around a focused, timely theme, demonstrating the growing recognition of the importance of collaborative healthcare education.
Future healthcare education should focus on:
- Optimizing resource utilization through strategic sharing
- Developing robust interprofessional competencies
- Creating sustainable financial models
- Continuously evaluating and improving patient care outcomes
By addressing these challenges and leveraging the advantages of both separate and integrated educational approaches, healthcare education can better prepare professionals for the collaborative, patient-centered care required in modern healthcare systems.
References
- BMC Medical Education. (2025). A scoping review of interprofessional education in healthcare: evaluating competency development, educational outcomes and challenges. Retrieved from https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-06969-3
- Interprofessional Education Collaborative. (2025). IPEC Core Competencies. Retrieved from https://www.ipecollaborative.org/ipec-core-competencies
- Journal of Interprofessional Care. (2025). Interprofessional attitudes of healthcare students: translation into Italian, validity, and reliability. Retrieved from https://www.tandfonline.com/doi/full/10.1080/13561820.2025.2495019
- NCBI Bookshelf. (2020). Costs and Financing of Health Professions Education. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK216015/
- PMC. (2019). Interprofessional education: effects on professional practice and healthcare outcomes. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6513239/
- American Interprofessional Health Collaborative. (2025). Collaborating Across Borders. Retrieved from https://aihc-us.org/activities/cab
- Texas A&M Health Science Center. (2025). Why is Interprofessional Education important in the health sciences? Retrieved from https://health.tamu.edu/iper/why.html



